Translate this page into:
Management of chronic spontaneous urticaria: Real-world Indian perspective
*Corresponding author: Dhiraj Dhoot, Global Medical Affairs, Glenmark Pharmaceuticals Ltd, Mumbai, Maharashtra, India. dhiraj.dhoot@glenmarkpharma.com
-
Received: ,
Accepted: ,
How to cite this article: Godse K, De A, Shah B, Girdhar M, Shankar K, Sarda A, et al. Management of chronic spontaneous urticaria: Real world Indian perspective. Indian J Skin Allergy 2022;1:11-6.
Abstract
Objectives:
There are multiple guidelines for chronic spontaneous urticaria (CSU) by various dermatological associations, but in real-world practice in India, different approaches have been noted. In this paper, we courted to determine these different approaches in CSU management, adherence to various CSU guidelines, and the reasons for deviation from guidelines amidst dermatologists in India.
Materials and Methods:
A net-based questionnaire was created and validated by five panelists experienced in CSU management and then was circulated to all dermatologists in India in August 2020 for real-world management scenario.
Results:
We received 880 completed response out of 2235 response. Most of the dermatologists (97%) were aware of some urticaria guidelines. Although many of them follow guidelines about three forth of them reported to deviate from it sometimes. The most common reason for deviation was rely on clinical experience as opted by 53% of respondents. Dermatologists who follow guidelines also investigate routinely in terms of complete blood count, the erythrocyte sedimentation rate, and thyroid-stimulating hormone as compared to those who do not. About 70.5% of the dermatologist prescribe second-generation antihistamine (SGAH) at approved dose as the first line of treatment whereas 63.6% up dose it as second line of treatment. Surprisingly, 68% prescribe first-generation antihistamine in the evening and SGAH in the morning as combination therapy in CSU.
Conclusion:
From the findings of the present study, it can be strongly implied that guidelines play a vital role in delivering superior attributes of patient care although 75% of dermatologists deviated from it. Main reasons for deviance are reliability on self-clinical proficiency and consideration of economic impediments. Both these factors need to be worked upon by continuous medical education of dermatologists and more pharmaco-economic research.
Keywords
India
Chronic spontaneous urticaria
Guidelines
Management
Adherence
INTRODUCTION
Chronic spontaneous urticaria (CSU), a mast cell-mediated disease is characterized by wheals and angioedema, or both for more than 6 weeks.[1,2] Prevalence of CSU is about 22% with a point prevalence of 1%[3-5] and it exerts a devastating impact on patients’ day-to-day life.[6,7] Although there are guidelines developed by many international as well as national associations, discrepancies between these guidelines create differences in diagnostic workup and management of CSU.[1,8,9] Additionally, many questions such as knowledge of the dermatologist regarding guidelines, its practical use in clinical practice, reasons for deviation from guidelines are left unanswered. Hence, further research is required to understand the real-world impact of these guidelines on the diagnosis of CSU and betterment of management strategy further leading to updation of guidelines and better patient care.
Skin Allergy Research Society of India developed a web-based questionnaire pertaining to knowledge of various CSU guidelines, reasons for deviation from the guidelines, and real-world office practice regarding CSU management. This survey was targeted to dermatologists in India since they are largely involved in the management of CSU.
MATERIALS AND METHODS
To determine the real-world practice on management of CSU, an expert panel comprising of 5 dermatologists with 15 years’ experience along with a research background in the field of CSU was created.
A net-based questionnaire was created and validated by five panelists and then was circulated to all dermatologists in India in August 2020 for real-world management scenario. A questionnaire composed of total of 20 questions related to awareness, adherence & alteration from CSU guidelines, laboratory work-up in CSU, and treatment options used. A reminder to participate was sent in September-October 2020. To reply, participants were given 15 days and complete anonymity was guaranteed.
RESULTS
Out of 2235 dermatologists from India, we received 880 (39.3%) completed surveys. Most of the dermatologists (70.5%) reported to have clinical experience of more than 10 years.
Urticaria guidelines
Majority of the dermatologists generally abide by theurticaria guidelines, whereas 74% of them diverge occasionally
Vast majority of the dermatologists (96.6%) were privy to one or more guidelines of urticarial management. Most of these dermatologists followed the guideline/s in their clinical practice. Amongst all the guidelines, the EAACI/GA2LEN/ EDF/WAO urticaria guideline[1] (55.7%) topped the list, followed by the Indian guideline (42%) and American AAAAI/ACAAI Joint Task Force practice parameters[9] (21.6%). About 18.2% of the dermatologist follow some other guidelines. Three fourth (74.12%) of the dermatologists deviate from the guideline/s which they usually follow.
Most common motive for non-following/deviation fromguidelines/s is more reliability of on self-clinical proficiency
352 (53.4%) respondents (out of 660 [75%]) conveyed that the most common reason for not following/deviating from following a guideline is more reliability on self-clinical proficiency. The second most common motive for diverging from these guidelines (14.8%) was marked as discouraging clinical outcomes after following it. All other reasons are detailed in Figure 1.
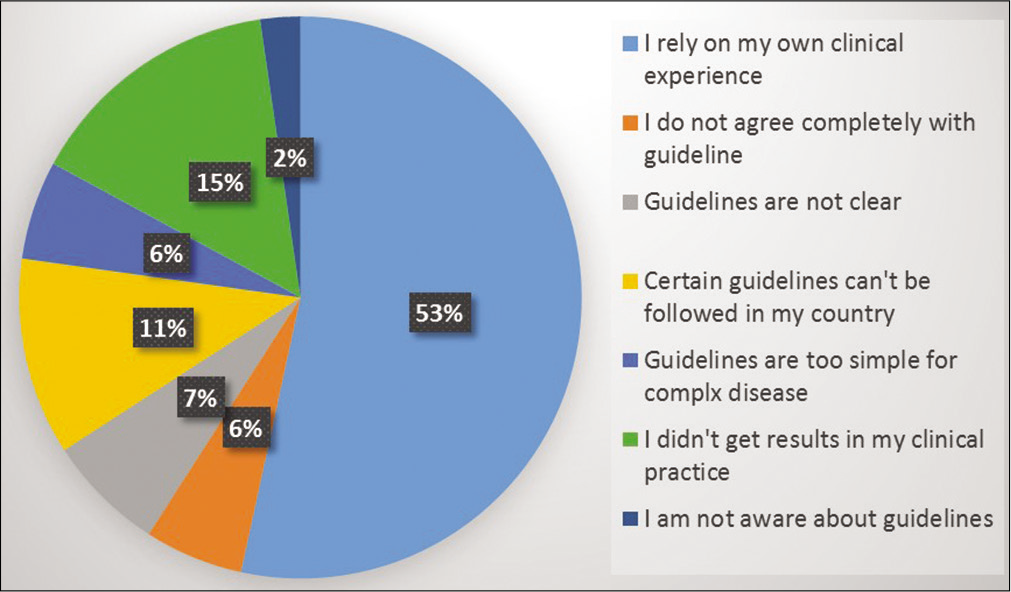
- Reasons for deviation from guideline.
Ordering diagnostic investigations more by dermatologistswho abide by urticarial guidelines/s
The frequency of requisitioning diagnostic tests such as erythrocyte sedimentation rate (ESR), complete blood count (CBC) was done regularly by the dermatologists who followed urticarial guideline/s [Figure 2]. About 76.2% advise dietary restriction.
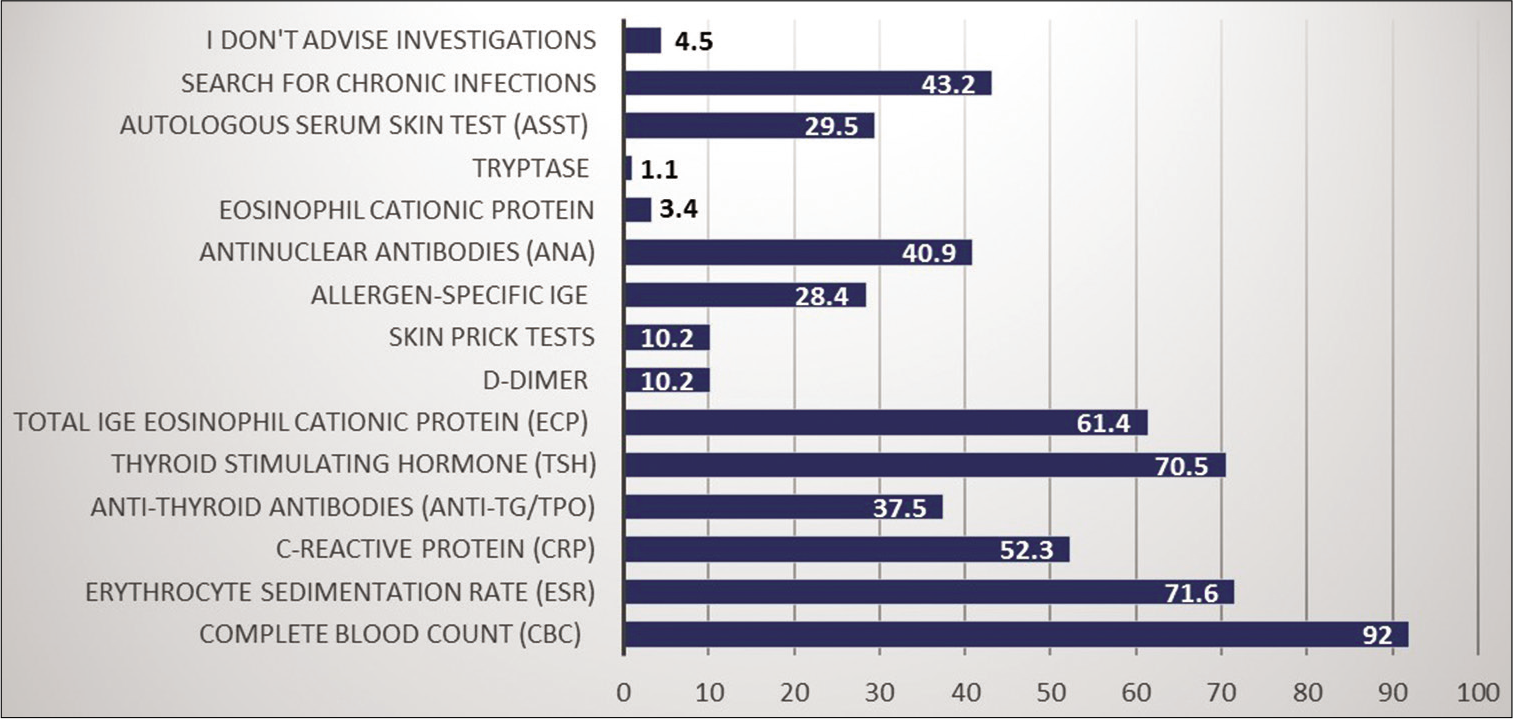
- Laboratory tests in chronic spontaneous urticaria.
Reliability on second-generation antihistamines (SGAH) and their increased prescribing trend is correlated with abidance to guideline/s of diagnosis and management of urticaria
About 70.5% of the dermatologist prescribe SGAH at standard dose as the first line of treatment whereas 63.6% up dose SGAH as the second line of treatment. Cyclosporine (25%) was commonly prescribed as the third line of treatment option [Figure 3]. First-generation anti-histamines (FGAH) were also commonly prescribed by 79.5% of the dermatologists in any phase of CSU management. The reasons behind prescribing FGAH were reported as unsatisfactory response to SGAH (73.9%), unavailability of SGAH (17%), and patients with laryngeal edema and anaphylactic shock (9.1%). Hydroxyzine was most commonly prescribed FGAH (69.3%) whereas 50% of dermatologist favor levocetirizine as SGAH [Figure 4]. Surprisingly, 68.2% prescribe FGAH in the evening and second generation in the morning as combination therapy in CSU.
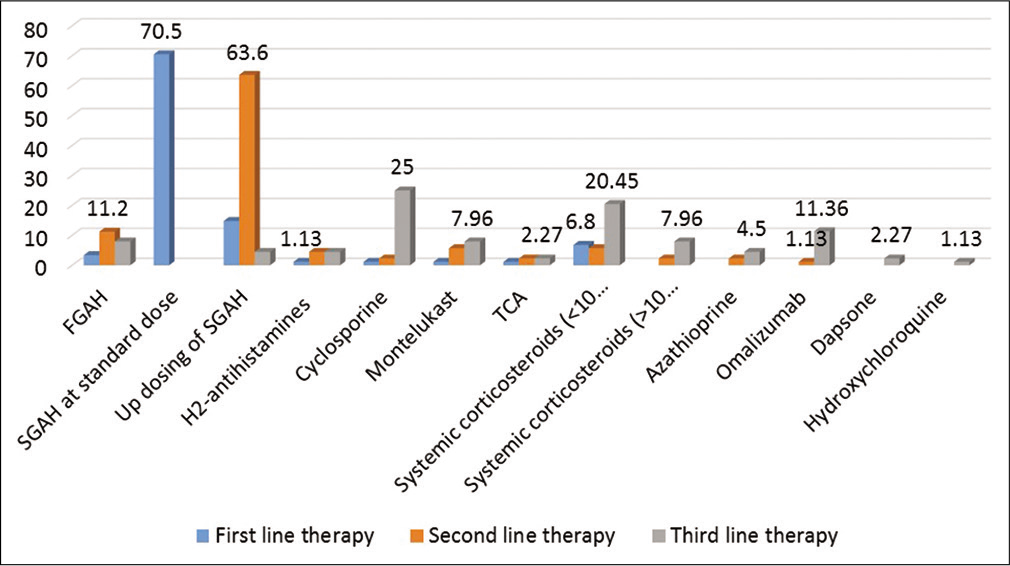
- Percentage of drugs prescribed in chronic spontaneous urticaria management at different levels.
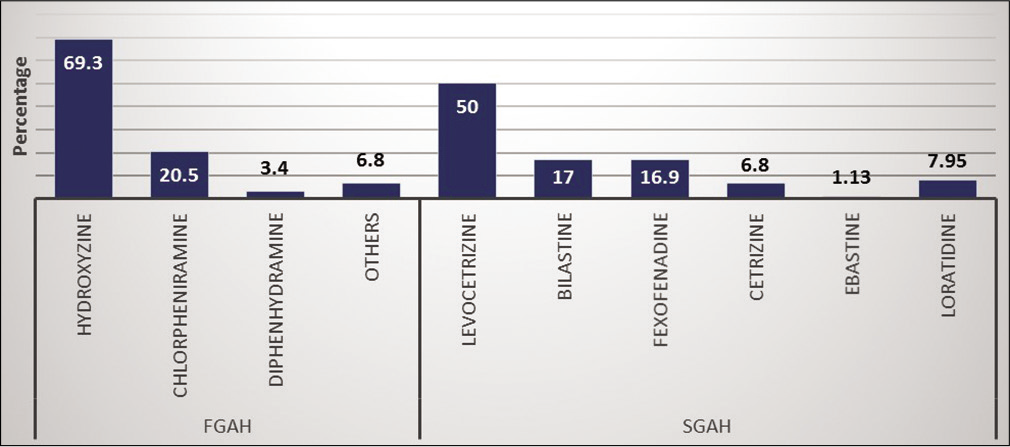
- Percentage of prescription of first and second generation antihistamine in chronic spontaneous urticaria.
Dermatologist often show confidence in other drugs
H2 antihistamines are prescribed by 84% of the dermatologists while montelukast by 72.7% in various phases of CSU management. Corticosteroids are also commonly used by 96.6% of dermatologist up to the dose of 0.5 mg/kg/day for less than 10 days (92% response). Reasons for corticosteroids use were reported as; (a) unsatisfactory response with antihistamines and other medications (27.3%); (b) patients with Laryngeal edema or anaphylaxis (30.7%); (c) adverse effects of long term antihistamines (1%); (d) for immediate and early relief of symptoms (33%) and (e) to shorten the duration of flares (8%). About 75% of dermatologists reported negative experience with omalizumab and reasons for the same are cited in Figure 5. Of the remaining, 63.7% prescribe omalizumab for 3–6 months.

- Reasons for not prescribing omalizumab.
Various immunomodulators were also quite commonly used in CSU as shown in Figure 6 and cyclosporine was the most popular immunomodulator as reported by 76.1% of respondents. It was commonly prescribed at the dose up to 3 mg/kg/day in CSU.
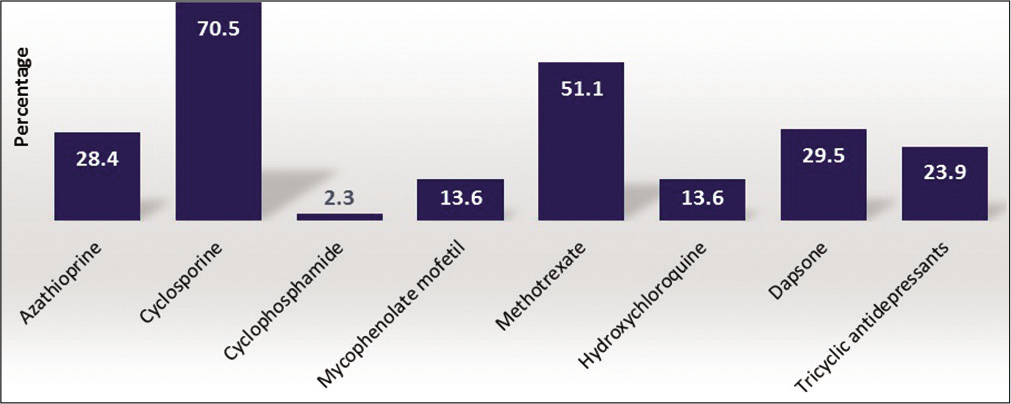
- Prescription percentage of other drugs in chronic spontaneous urticaria.
DISCUSSION
Past few recent years have witnessed advancement in the management of CSU via the formulation of plethora of consensus statements, guidelines, etc. Few researchers have done countrywide studies to analyze the awareness of dermatologists to urticarial management guidelines/s and the actual inculcation of these guidelines in clinical practice.[10,11] To the best of our knowledge, this is the first study that examined the real-world management of CSU in India.
Majority of the dermatologists are aware and abide by urticaria guidelines in the management of their patients
Almost all dermatologists had knowledge of urticaria guideline/s and its adherence in their clinical practice. Although this is in concordance with a recently published survey on CSU management[2] there is irregularity when the present study was compared with other studies done in different parts of the globe. Only one-fifth of physicians in a study done at Ecuador had the awareness about GA2LEN/ WAO/EAACI/EDF urticaria guideline/s.[10] Similarly, only 33% of the physicians in a German study had knowledge of these guideline/s.[11] These findings were corroborated in an Italian study, wherein a little above half of the physicians were aware about urticarial guideline/s, and only quarter of these abided by the guideline/s in clinical practice.[12] In the present study, augmented rate of compliance with urticaria guideline/s can be attributed to surge in acknowledgment of participants to these guidelines/s. Second attributable factor for this finding is that all the respondents in the present study were dermatologists.
Reasons for non-adherence or alteration from CSU guidelines
Although >90% follow some guidelines, about 75% of them deviate from it sometimes. Confidence on the self-experience of clinical practice was the most common factor stated for this (53%). This need gap can be filled by creating means to raise awareness of dermatologists about pros of abiding to these guidelines in clinical practice. Moreover, it is the need of the hour to edify dermatologists that guidelines are designed to augment clinical decision making and not a locum for it.
About 11% of dermatologist reported that few recommendations from these guidelines are not feasible for clinical practice in India. In real-world Indian setting, economy of the patient plays a vital role in designing any form of therapeutic strategy. For example, omalizumab is less prescribed in India due to high cost or non-insurance cover. FGAH are commonly prescribed due to easy availability and cost-effectiveness. Hence, it is prudent to consider cost-effectiveness of treatment strategy in developing countries like India.
A worldwide council of experts in the field of CSU revise the EAACI/GA2LEN/EDF/WAO guidelines in a duration of 4 years apart. Curiously, 7% of dermatologist perceived that there is a lack of clarity in recommendations of these guidelines or they do not harmonize with it. This points out to the need for contemplation of corrections in the formulation of amendments and advancement of these guidelines. There is minimal difference in recommendations given by all of urticaria guidelines. For instance, practice parameters in the United States endorse use of H2 antihistamines as second-line and FGAH as third-line drugs in the management of urticaria, in contrast to the EAACI/GA2LEN/EDF/WAO guidelines.[13] In case of patients non-responsive to SGAH at standard dose, Japanese guidelines recommend either switching to other H1-antihistamines or combined use or increasing the dose of antihistamine.[14] The reason for not adhering to guideline/s was stated as disparity between various guidelines by 6% of the study participants.
On collation, faith on self-clinical proficiency appears to be the major factor for non-adherence/deviance from guidelines/s. Surprisingly, unavailability of drugs/economic constraint was not marked as major factor responsible for this finding. This observation endeavors the tussle among experience and evidence-based medicine which directs us to impart medical education to dermatologists in an ongoing manner.
Impact on diagnostic tests
CBC, ESR, and C reactive protein are the usual investigations for patients of CSU as recommended by WAO/EDF/EAACI/ GA2LEN.[1] The US guidelines additionally recommend monitoring of liver enzymes and TSH parameters.[9] As per anticipation, these investigations were ordered more commonly by dermatologists in India as seen with other surveys.[10,11] Interestingly, most of the participants reported to implement various diagnostic measures to do so.
In pursuit of excluding other differential diagnostic possibilities, supplementary investigations are reserved as a part of protracted diagnostic strategy.[1] For example, Serum eosinophil cationic protein (ECP) can be a better indicator of disease severity in CSU than IgE, and patients with high ECP levels from the beginning require a relatively longer duration of therapy and can be managed by more than two different kinds of oral antihistamines.[15] In our survey, 61% responded for ECP and 28% for IgE. In one cross-sectional study from Latin America, 83.5% responded for IgE.[10] Interestingly, 43% of respondents perform investigations to rule out other chronic diseases.
IgG autoantibodies against IgE and its receptors on basophils and mast cells are found in half of the patients with CSU.[16] Autoreactive CSU is one of the most frequent subtypes of the disease[17] and 29% of respondents carried out ASST which is not in concordance with other surveys.[11]
Quality of care: Impact of the CSU guidelines
All the urticaria guidelines recommend in unison[1,9,18] that the first line of therapy should be SGAH at a licensed dose which was reflected in our survey as well. This finding was corroborated by a cross-sectional observational study, wherein SGAHs were the most commonly prescribed drugs in patients of CSU.[12,19]
The EDF/GA2LEN/EAACI/WAO urticaria guideline endorse the use of SGAH as second-line drugs in the management of CSU in high dose which can go up to 4 times the standard dose. In our survey also, 63% prescribe up dosing of SGAH as second line of therapy which in line with other reports.[11,12] Apart from that about 11% responded positively for FGAH as second line of management.
As per EDF/GA2LEN/EAACI/WAO guideline montelukast (US practice parameter-step 2) or omalizumab, cyclosporine (US practice parameter-step 4) as next therapeutic choice in patients who fail to respond to increased dose of SGAHs.[1,9] Interestingly, most of the dermatologists in spite of experience with other or alternative treatment options were not convinced regarding their use routinely. This is in line with report highlighting limited benefit of dapsone [20] and providing only limited or anecdotal supportive evidence for immunosuppressant.[21] Only for cyclosporine, there is substantial evidence available supporting its effectiveness in CSU.[22,23] In our survey, 25% reported to prescribe Cyclosporine whereas only 11% preferred omalizumab. Reasons behind not using omalizumab were cited as expensive drug and less experience with the same. Surprisingly, survey revealed the use of systemic corticosteroids by 20% of respondents. As per some reports, its short duration use has been found to be beneficial in refractory CSU.[24-26] In summary, owing to lack of comprehensive management options in CSU, there is a need for new and effective therapies.
Combination of first- and second-generation antihistamines
Since more than 40% of CSU patients do not respond to licensed dose of SGAH,[27] some guidelines suggest addition of a second antihistamine.[9,14] Although use of FGAH is alarmed in the European guideline,[1] but as per one report, 15% of the patients were managed with hydroxyzine at some time during their disease.[28] Moreover, after the failure of treatment with SGAH, successful use of FGAH has been described.[29] Same has been reflected in our survey where 68.2% reported the use of combination of FGAH in the evening and SGAH in the morning in CSU management with hydroxyzine being the most commonly prescribed FGAH. It could be due to recommendations by Indian guidelines[3] suggesting the use of hydroxyzine in non-responsive cases, ease of availability, cost-effectiveness, and vast experience of the Indian doctors using the molecule.
Limitations
In survey studies, the chances of selection bias cannot be ruled out. Although we did a survey with dermatologists only, the response rate was on the lower side (40%). However, this limitation is less likely to influence the character of our results.
CONCLUSION
From the findings of the present study, it can be strongly implied that guidelines pertaining to diagnosis and management of urticaria play a vital role in delivering superior attributes of patient care. One of the significant findings of the present study was that although most dermatologists followed urticaria guideline/s, 75% of them deviated from it. Two common factors which can be cogitated for such deviance are reliability on self-clinical proficiency and the resultant lack of will to fully adhere to the recommendations made by the guidelines and consideration of economic impediments while updating/formulation of guidelines. Both these factors need to be worked upon by continuous medical education of dermatologists and more pharmaco-economic research.
Ideally, guidelines on the management of urticaria should enable dermatologist to customize treatment according to each patient as well as it should be updated covering existing gaps with augmented and effective propagation. It can be anticipated that this will help to improve clinical outcome, quality of life of patients, and avoidance of unfitting treatment strategies.
Acknowledgments
We would like to acknowledge our sincere gratitude to the global medical services of Glenmark Pharmaceuticals Limited for their help in data collation, analysis, and preparation of the manuscript of this expert consensus. We also acknowledge dermatologists in India for participating in this survey.
Declaration of patient consent
Patient’s consent not required as there are no patients in this study.
Financial support and sponsorship
Nil.
Conflict of interest
Dr. Dhiraj Dhoot and Dr. Hanmant Barkate are employees of Glenmark Pharmaceuticals Ltd, India. None of the authors have any conflicts of interest to declare.
References
- The EAACI/GA2LEN/EDF/WAO guideline for the definition, classification, diagnosis and management of urticaria. Allergy. 2018;73:1393-414.
- [CrossRef] [PubMed] [Google Scholar]
- Management of chronic spontaneous urticaria: A worldwide perspective. World Allergy Organ J. 2018;11:14.
- [CrossRef] [PubMed] [Google Scholar]
- Consensus statement for the diagnosis and treatment of urticaria: A 2017 update. Indian J Dermatol. 2018;63:2-15.
- [CrossRef] [PubMed] [Google Scholar]
- Epidemiology of urticaria in Spain. J Investig Allergol Clin Immunol. 2004;14:214-20.
- [Google Scholar]
- Epidemiology of chronic spontaneous urticaria: Results from a nationwide, population-based study in Italy. Br J Dermatol. 2016;174:996-1004.
- [CrossRef] [PubMed] [Google Scholar]
- The impact of chronic urticaria on the quality of life. Br J Dermatol. 1997;136:197-201.
- [CrossRef] [PubMed] [Google Scholar]
- Unmet clinical needs in chronic spontaneous urticaria. A GA2 LEN task force report. Allergy. 2011;66:317-30.
- [CrossRef] [PubMed] [Google Scholar]
- Urticaria guidelines: Consensus and controversies in the European and American guidelines. Curr Allergy Asthma Rep. 2015;15:30.
- [CrossRef] [PubMed] [Google Scholar]
- The diagnosis and management of acute and chronic urticaria: 2014 update. J Allergy Clin Immunol. 2014;133:1270-7.
- [CrossRef] [PubMed] [Google Scholar]
- Knowledge and management of chronic spontaneous urticaria in Latin America: A cross-sectional study in Ecuador. World Allergy Organ J. 2017;10:21.
- [CrossRef] [PubMed] [Google Scholar]
- Management of chronic spontaneous urticaria in real life-in accordance with the guidelines? A cross-sectional physician-based survey study. J Eur Acad Dermatol Venereol. 2013;27:43-50.
- [CrossRef] [PubMed] [Google Scholar]
- State of the art of chronic spontaneous urticaria in Italy: A multicentre survey to evaluate physicians' and patients' perspectives. BMJ Open. 2016;6:e012378.
- [CrossRef] [PubMed] [Google Scholar]
- A review of international recommendations for the diagnosis and management of chronic urticaria. Acta Derm Venereol. 2017;97:149-58.
- [CrossRef] [PubMed] [Google Scholar]
- Japanese guidelines for diagnosis and treatment of urticaria. Arerugi. 2017;66:23-6.
- [Google Scholar]
- Eosinophil Cationic Protein in Chronic Urticaria. Intern Med. 2012;2:112.
- [CrossRef] [Google Scholar]
- Autoimmune chronic spontaneous urticaria: What we know and what we do not know. J Allergy Clin Immunol. 2017;139:1772-81.e1.
- [CrossRef] [PubMed] [Google Scholar]
- General practitioners, dermatologists, allergists, and the management of chronic urticaria. Results of a practice survey. Ann Dermatol Venereol. 2003;130(1):S160-73.
- [Google Scholar]
- Chronic urticaria: A comparison of management guidelines. Expert Opin Pharmacother. 2011;12:2683-93.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic urticaria: Do urticaria nonexperts implement treatment guidelines? A survey of adherence to published guidelines by nonexperts. Br J Dermatol. 2009;160:823-7.
- [CrossRef] [PubMed] [Google Scholar]
- Prospective randomized non-blinded clinical trial on the use of dapsone plus antihistamine vs antihistamine in patients with chronic idiopathic urticaria. J Eur Acad Dermatol Venereol. 2008;22:481-6.
- [CrossRef] [PubMed] [Google Scholar]
- Chronic urticaria: Aetiology, management and current and future treatment options. Drugs. 2004;64:2515-36.
- [CrossRef] [PubMed] [Google Scholar]
- Cyclosporine in chronic idiopathic urticaria: A double-blind, randomized, placebo-controlled trial. J Am Acad Dermatol. 2006;55:705-9.
- [CrossRef] [PubMed] [Google Scholar]
- Cyclosporine-A in severe chronic urticaria: The option for long-term therapy. Allergy. 2010;65:1478-82.
- [CrossRef] [PubMed] [Google Scholar]
- Usefulness of a short course of oral prednisone in antihistamine-resistant chronic urticaria: A retrospective analysis. J Investig Allergol Clin Immunol. 2010;20:386-90.
- [Google Scholar]
- Severe chronic urticaria treated with oral mini-pulse steroid therapy. Indian J Dermatol. 2010;55:402-3.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of refractory chronic urticaria: Current and future therapeutic options. Am J Clin Dermatol. 2013;14:481-8.
- [CrossRef] [PubMed] [Google Scholar]
- Updosing nonsedating antihistamines in patients with chronic spontaneous urticaria: A systematic review and meta-analysis. Br J Dermatol. 2016;175:1153-65.
- [CrossRef] [PubMed] [Google Scholar]
- Effectiveness and safety of antihistamines up to fourfold or higher in treatment of chronic spontaneous urticaria. Clin Transl Allergy. 2017;7:4.
- [CrossRef] [PubMed] [Google Scholar]
- What the first 10, 000 patients with chronic urticaria have taught me: A personal journey. J Allergy Clin Immunol. 2009;123:713-7.
- [CrossRef] [PubMed] [Google Scholar]






