Translate this page into:
Symmetrical drug-related intertriginous and flexural exanthema without baboon syndrome due to paracetamol: An uncommon side effect of a common drug: A case report and a review of literature
*Corresponding author: Rinki Tayal, Department of Dermatology, Era’s Lucknow Medical College and Hospital, Lucknow, Uttar Pradesh, India. tayalrinki1996@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Tayal R, Khatri N, Siddiqui MA. Symmetrical drug-related intertriginous and flexural exanthema without baboon syndrome due to paracetamol: An uncommon side effect of a common drug: A case report and a review of literature. Indian J Skin Allergy. 2024;3:138-40. doi: 10.25259/IJSA_30_2024
Dear Editor,
The term symmetrical drug related intertriginous and flexural exanthema (SDRIFE) refers to a specific clinical pattern of drug eruption caused by systemic exposure to a drug. It manifests as well-defined rashes over intertriginous areas, intergluteal clefts, and/or upper thighs. SDRIFE and Baboon syndrome were used synonymously previously. However, recently, these have been separated, as SDRIFE does not involve buttocks, and previous sensitization is not necessary, both of which are seen in baboon syndrome.[1] Various medications have been implicated as a cause, including beta-lactam antibiotics, antifungals, analgesics including paracetamol. SDRIFE is often a type IV hypersensitivity reaction that develops 2 – 3 days after initial exposure to the drug/allergen in sensitized patients and after 9 – 10 days in non-sensitized patients.[2] The histopathological findings are non-specific and show eczematous features such as variable spongiosis and upper dermal infiltrates of mononuclear cells, including eosinophils.[3] SDRIFE is an uncommon side effect of paracetamol. We present here a case of a young male who developed features of SDRIFE following paracetamol ingestion.
A 29-year-old male presented to the outpatient department with multiple red-colored patches over his body. These developed 1 day after taking a single dose of oral paracetamol 500 mg. These lesions initially appeared on bilateral forearms and gradually progressed to involve the chest, back, bilateral thighs, and groins within the next 1 day, associated with intense itching. There was no history of any other drug intake, topical application, or exposure to irritants. The Naranjo probability scale revealed a probable adverse drug reaction to paracetamol.
On examination, there were present multiple, well-defined, symmetric, livid to erythematous maculopapular exanthems over the axillae and adjacent areas of the upper chest and back, bilateral cubital fossa, and inguinal folds, completely sparing the gluteal region. Examination of hair, nails, genital, and oral mucosa revealed no abnormality. Systemic examination was within normal limits [Figures 1 and 2]. Histopathological examination from a representative lesion showed spongiosis and superficial perivascular inflammatory infiltrate composed mostly of lymphocytes and occasional neutrophils. There was papillary dermal edema with sparse intraepidermal eosinophils. Incontinence of black pigment granules was also seen [Figure 3]. Hence, a diagnosis of SDRIFE without baboon syndrome caused by paracetamol was made. The patient was asked to avoid paracetamol in the future and was prescribed topical mild corticosteroids and antihistamines. The lesions resolved completely after 5 days [Figure 4].

- Symmetrical maculopapular erythematous rash over bilateral (B/L) axilla, upper back, and flanks.

- Symmetrical maculopapular erythematous rash over bilateral (B/L) cubital fossae, arms, and axilla.
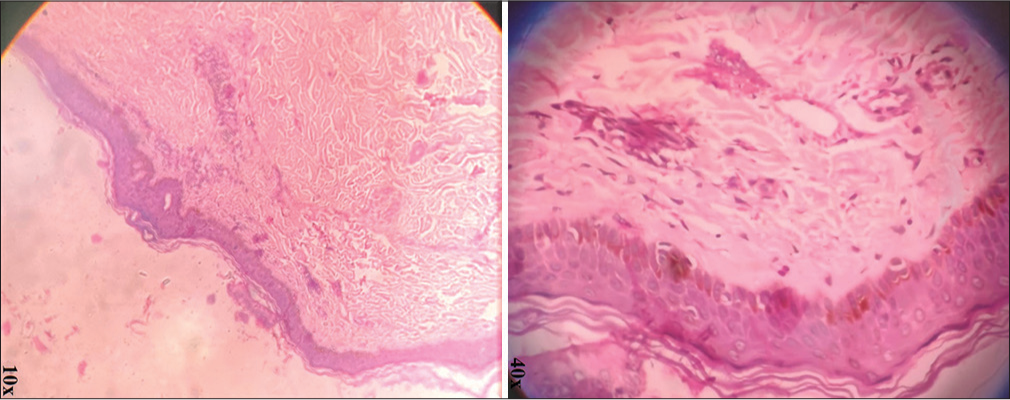
- Hematoxylin and eosin (H&E) stained section (× 10 and × 40) showing spongiosis, superficial perivascular inflammatory infiltrate composed mostly of lymphocytes and occasional neutrophils, papillary dermal edema with sparse intraepidermal eosinophils and incontinence of black pigment granules.

- Resolution of lesions after 5 days.
SDRIFE is a benign and self-limiting drug eruption. It is characterized by symmetrical involvement of gluteal and intertriginous areas. A possible reason for this distribution appears to be the preferential trafficking of activated memory T-cells in these areas, which is a type of recall phenomenon after a past physical/inflammatory insult. This occurs due to Type 4 hypersensitivity reaction to a number of drugs.[1] Drugs commonly causing SDRIFE include beta-lactam antibiotics (penicillin, especially amoxicillin, and cephalosporins), uncommonly non-beta lactams, antifungals, iodine-containing contrast agents, analgesics, and infliximab.[4] Classical histopathological findings include focal spongiosis, a mixed dermal infiltrate of neutrophils and CD3+T lymphocytes, as well as macrophages and plasma cells. Interphase dermatitis, basal cell vacuolization, and necrotic keratinocytes are occasionally seen.[3] Treatment is mainly symptomatic. The offending drug should be withdrawn and avoided in the future. Topical/systemic steroids may hasten resolution. Lugović-Mihić et al., in 2013, reported a case of a 33-year-old male who presented with SDRIFE with Baboon syndrome after 24 h of ingestion of a single dose of paracetamol 500 mg.[5] Our case is different from theirs as the involvement of buttocks was not seen. We could not find any other previous reports with similar presentations.
Paracetamol is the most commonly prescribed non-steroidal anti-inflammatory drug and the most common “over-the-counter” antipyretic and analgesic. We report this case to highlight the possible development of SDRIFE as an uncommon side effect of paracetamol. This indicates the need for a high index of suspicion that will enable early diagnosis and prevent unnecessary invasive investigations and treatment.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil.
References
- Symmetric drug-related intertriginous and flexural exanthema due to itraconazole: An uncommon side effect of a commonly used drug. Indian Dermatol Online J. 2017;8:501-3.
- [CrossRef] [PubMed] [Google Scholar]
- Baboon syndrome resulting from systemic drugs: Is there strife between SDRIFE and allergic contact dermatitis syndrome? Contact Dermatitis. 2004;51:297-310.
- [CrossRef] [PubMed] [Google Scholar]
- Symmetrical drug-related intertriginous and flexural exanthema (SDRIFE) associated with pristinamycin, secnidazole, and nefopam, with a review of the literature. Contact Dermatitis. 2018;79:378-80.
- [CrossRef] [PubMed] [Google Scholar]
- Pustulobullous variant of SDRIFE (symmetrical drug-related intertriginous and flexural exanthema) J Dtsch Dermatol Ges. 2017;15:657-9.
- [CrossRef] [Google Scholar]
- SDRIFE (baboon syndrome) due to paracetamol: Case report. Acta Dermatovenerol Croat. 2013;21:113-7.
- [Google Scholar]





