Translate this page into:
Stem-cell therapy in dermatology – Challenges and opportunities
*Corresponding author: Abhishek De, Associate Professor, Department of Dermatology, Calcutta National Medical College and Hospital, Kolkata, West Bengal, India. dr_abhishek_de@yahoo.co.in
-
Received: ,
Accepted: ,
How to cite this article: Chakraborty D, De A. Stem-cell therapy in dermatology – Challenges and opportunities. Indian J Skin Allergy. 2024;3:93-105. doi: 10.25259/IJSA_50_2023
Abstract
The remarkable characteristics of stem cells (SCs), particularly their potency, capacity for self-renewal, and clonality, are well known. In recent years, there have been notable advancements in the field of cell therapy. Due to its distinctive qualities and versatility, this innovative therapy is already turning into a potentially helpful remedy for several diseases. Numerous dermatological problems, including autoimmune skin disorders, atopic dermatitis, skin aging, wound healing, scar repair, and many more, have been treated with SC-based therapies. Their application in regenerative medicine and esthetic dermatology is based on their capacity to self-renew and differentiate into distinct cell types. Given their abundance and relative simplicity of collecting adipose-derived SCs have shown to be particularly appealing in terms of appearance. SC therapy has demonstrated encouraging results in both skin regeneration and androgenetic alopecia treatment. Despite favorable preclinical evidence and clinical investigations, further randomized, controlled trials and treatment standardization are required to fully comprehend the role of SCs in the treatment of dermatological conditions, especially esthetics. The purpose of this article is to provide a general review of cell-based therapy, including its current uses, limits, and future possibilities in the field of dermatology.
Keywords
Stem cells
Regenerative medicine
Cellular therapy
Skin rejuvenation
Dermatological treatment
INTRODUCTION
Modern medicine emphasizes two key aspects that did not receive much attention previously. One of them is disease prevention, and the other is regenerative medicine. While the first one aims to prolong a patient’s life span by preventing the disease from occurring, the second is an effort to treat diseases for which there is currently no solution.[1] Stem-cell (SC) therapy is a part of regenerative medicine and has been used for a wide range of therapeutic indications. The principles by which Mario R. Capecchi and his team used embryonic SCs to alter mice’s genes precisely made it possible to modify the germline of mammals and produce offspring that express the altered gene, earning them the 2007 Nobel Prize in Physiology.[2] Over the years, SC therapy has been used in dermatology for a number of refractory diseases with some success. An overview of SC therapy’s history, current uses in dermatology, and possible applications in the future are all intended to be covered in this article.
SEARCH STRATEGY
Using both Medical Subject Headings (MeSH) and non-MeSH keywords, a thorough, complete, strategic electronic search of the PubMed, Scopus, Medline, Google Scholar, and EBSCO databases over the period 2004–2023 was conducted. Keywords included “stem-cell therapy” AND “Dermatology,” OR “mesenchymal,” OR “hematopoietic,” “allogenic,” OR “autologous,” “inflammatory skin diseases,” OR “cutaneous malignancies,” “wound healing” OR “therapy,” OR “esthetic.” Two reviewing authors analyzed and extracted the data from the searches. The references of extracted articles were also scanned for additional information to compile this narrative review, as shown in Figure 1.
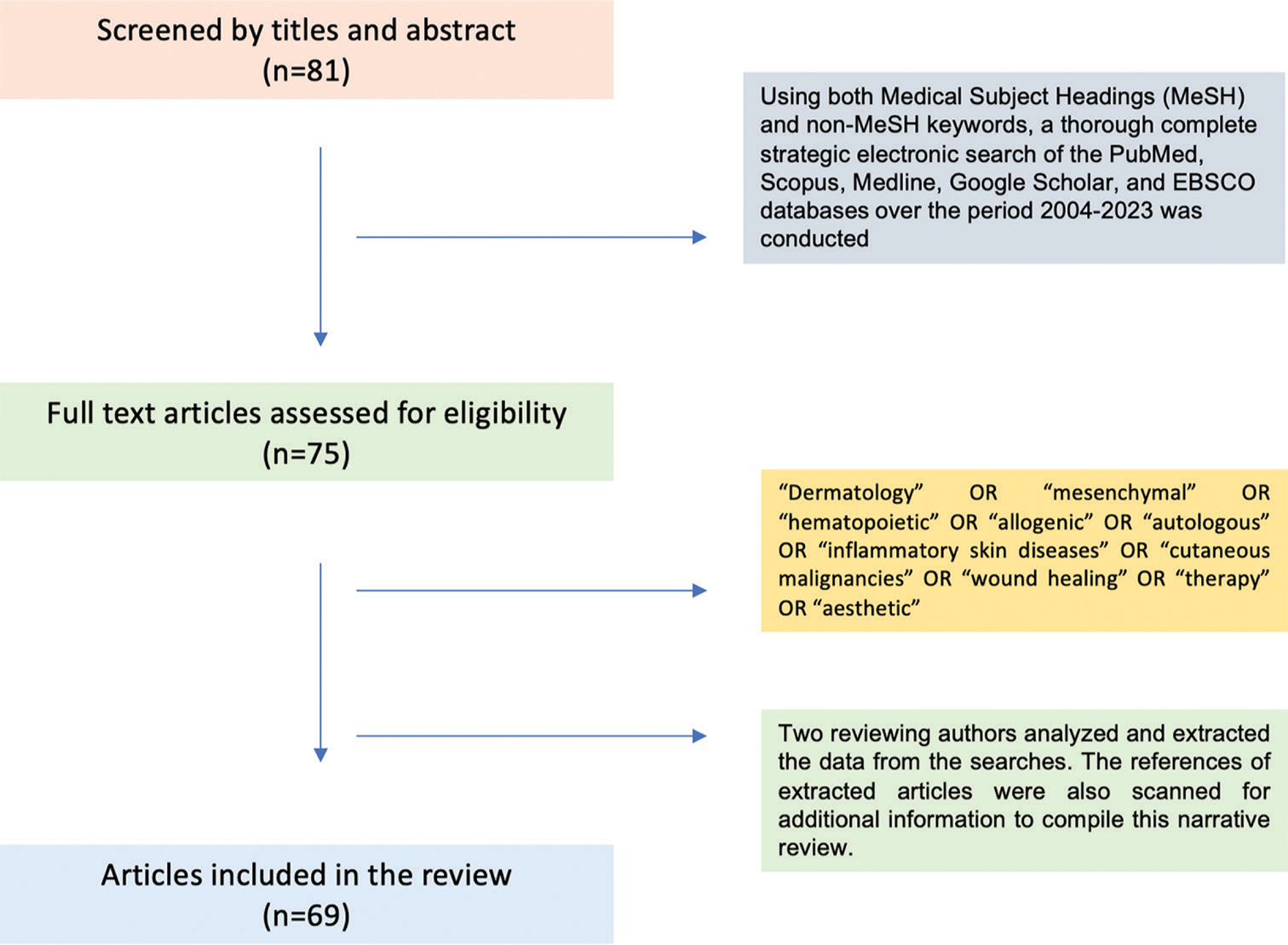
- Flow chart of the search strategy, EBSCO: Elton B. Stephens Company
SCs IN SKIN AND THEIR ROLE IN TISSUE REGENERATION
SCs are abundant in the skin since they replicate rapidly. Near the basal membrane are epidermal interfollicular SCs, which heal epidermal injuries. Hair follicles have follicular, sebaceous, and neural crest SCs. The bulge includes follicular and neural crest SCs. Sebaceous glands also contain SCs. Mesenchymal SCs (MSCs) are there in the hypodermis, adipose tissue, and dermis. They produce fibroblasts and myofibroblasts, which repair and regenerate soft tissue and musculoskeletal and vascular systems. Since melanocyte SCs may be triggered by ultraviolet (UV) light, lasers, dermabrasion, and drugs like tacrolimus, they can be utilized to re-pigment vitiligo. Normally, SCs from the epidermis, sebaceous glands, and hair follicles differentiate independently of each other. However, during injury due to its plasticity, SCs from any location can generate an entire cell lineage.[3]
Skin SCs are abundant, easy to acquire, and autologous, preventing graft-versus-host disease (GvHD). Animal and in vitro experiments have shown the potential and adaptability of cutaneous SCC. Human dermal MSCs have demonstrated a strong capacity for growth in vitro, particularly when taken from neonates. Their easy acquisition, proliferation, and security, as shown by population doublings in culture, suggest they may be effective for adipose, muscular, and osteogenic tissue regeneration.[4] Dermal fibroblasts have undergone genetic modification in vitro since 2006 to regress to a pre-differentiated state. They were then encouraged to develop into separate cell lines. In vitro, fibroblast regression creates induced pluripotent stem cells (iPSCs). We refer to MSCs found in adipose tissue’s stromal vascular fraction (SVF) as adipose tissue-derived stem cells (ADSCs). ADSCs become adipogenic, myogenic, chondrogenic, and osteogenic in vitro. They are easy to collect and plentiful, making them popular for esthetic indications.[5]
There is still no clear pattern that can specify the relative importance of each cell in the skin regeneration process in relation to the others. However, it is generally recognized that there are important molecular links between systems; for example, dermal fibroblasts and hypodermis cells function in a paracrine manner. Because they coordinate the response to tissue repair by activating growth factors, extracellular matrix secretory proteins, and other host cells, MSCs are essential to this process.[6] The basic classification of SCs is shown in Table 1.[7] However, it can also be classified as per utility, as shown in Table 2.[7]
| Parameter | Type of cell | Characteristics |
|---|---|---|
| Origin | Embryonic | Pluripotent cells that arise from the inner cell mass of the blastocyst. |
| Fetal | Multipotent cells are classified further according to the cells they generate (hematopoietic, neural, mesenchymal, endothelial, and epithelial) | |
| Somatic | It is derived from placenta and adult tissue and may be either unipotent or oligopotent. | |
| Induced pluripotent | Somatic stem cells that have been artificially reprogrammed to have characteristics of embryonic stem cells, including pluripotency, are known as induced pluripotent stem cells. | |
| Differential potential | Totipotent | Maximum potential for distinction. It develops into extra-embryonic and embryonic tissues and provides the seed for pluripotent cells. |
| Pluripotent | Able to develop into cells that come from the endoderm, ectoderm, and mesoderm germ layers, but not extra-embryonic tissues | |
| Multipotent | Restricted ability to differentiate. Only gives rise to cells that are members of particular lineages, such as hematopoietic and brain stem cells. | |
| Oligopotent | Produces many cells, such as myeloid stem cells, inside a single tissue. | |
| Unipotent | Lowest potential for differentiation because it consistently divides into a single kind of cell. |
Autoimmune Dermatoses
Autoinflammatory Dermatoses
Genetic Dermatoses
Wound Healing
Localized Dermatoses
Aging-related Dermatoses
|
SC: Stem cell, MSC: Mesenchymal stem cell, HSC: Hematopoietic stem cell, ADSCs: Adipose-derived stem cells, iPSCs: Induced pluripotent stem cells
APPLICATIONS OF SC THERAPY FOR TREATMENT OF DERMATOLOGICAL DISORDERS
Allergic diseases
Atopic dermatitis (AD)
Current treatment options for AD aim at symptom control and inflammation reduction, but they often lack long-term efficacy and have side effects. SC therapy has emerged as a promising new approach for AD management due to its immunomodulatory and regenerative properties.
SCs, particularly MSCs, exert therapeutic effects in AD through various mechanisms:
Immunomodulation: MSCs suppress overactive immune responses by inhibiting T-cell activation, decreasing proinflammatory cytokines, and promoting anti-inflammatory molecules.
Regeneration: MSCs differentiate into keratinocytes, fibroblasts, and endothelial cells, contributing to skin barrier repair and neovascularization.
Paracrine effects: MSCs secrete a multitude of growth factors and cytokines that promote tissue repair, angiogenesis, and anti-inflammatory responses.
MSCs can dampen both innate and adaptive immune systems, which shows that they have a therapeutic role in immune-related diseases, including AD. Again, MSCs may cause AD by upregulating T helper (Th)1/Th17 and downregulating Th2.
Preclinical studies utilizing MSCs in animal models of AD have demonstrated promising results, including reduced inflammation, improved skin barrier function, and decreased pruritus. Clinical trials investigating MSC therapy (MSCT) for AD are still in their early stages, with limited phase I and II studies showing potential benefits in terms of safety, tolerability, and efficacy. Several delivery routes are being explored for MSC administration in AD, including topical application, intralesional injection, and systemic infusion. Each route has its advantages and disadvantages, requiring further investigation to optimize delivery and improve therapeutic outcomes.
In mice, increased human umbilical blood-derived MSCs (huB-MSCs) reduced AD. The symptoms decrease due to the inhibition of mast cell degranulation and lymphocyte B-cell maturation by increased synthesis of prostaglandin E2 and tumor growth factor-b1 (TGF-b1). In addition, exosomes from adipose tissue-derived stem cells (ADSCs) can decrease proinflammatory cytokine expression, eosinophil count, and serum immunoglobulin E levels in animal models of AD. A recent two-phase clinical experiment using huB-MSCs yielded encouraging outcomes without life-threatening side effects. Since there is not enough data to state whether SC therapy can help improve AD, more studies need to be conducted.[8,9]
Despite the encouraging preclinical and early clinical data, several limitations and challenges need to be addressed for SC therapy to become a mainstream treatment for AD:
Heterogeneity of SCs: MSCs isolated from different sources show variable immunomodulatory and regenerative capacity, necessitating standardized isolation and culture protocols.
Dosage and timing: Determining the optimal dose and timing of SC administration is crucial for maximizing therapeutic benefit and minimizing potential side effects.
Safety concerns: Long-term safety data on the systemic administration of SCs is still limited, and potential risks such as tumorigenesis and immunogenicity need to be carefully evaluated.
Cost and scalability: SC therapy currently holds a high cost due to extensive laboratory processing and specialized personnel requirements. Optimizing production and delivery methods is essential for broader accessibility and affordability.
SC therapy holds immense potential for revolutionizing the management of AD. Preclinical and early clinical studies demonstrate promising results in terms of safety, tolerability, and efficacy. However, overcoming limitations related to SC heterogeneity, dosage optimization, safety considerations, and cost-effectiveness is crucial for successful clinical translation. Further, research with larger and well-designed clinical trials is necessary to establish the efficacy and safety of SC therapy as a viable treatment option for AD patients.
Chronic urticarial (CU)
In 2020, Özdemir et al.[10] conducted the first study of MSCT in humans with CU. This open-label and single-center clinical trial involved ten patients receiving autologous bone marrow-derived MSCs (BM-MSCs) and ten control patients. The MSCs were administered intravenously at a dose of 1 × 106 cells/kg twice, 2 weeks apart, with clinical follow-up for 6 months.
The study included patients with chronic spontaneous urticaria (CSU) for at least 1 year, who had not achieved disease control with omalizumab and cyclosporine for over 6 months, and who had a weekly urticaria activity score (UAS7) >20. Exclusions were those with chronic inducible urticaria, AD, other underlying itchy skin diseases, parasitic infections, or a history of malignancy.
MSCT was well tolerated with no reported adverse effects. Clinical responses were categorized as well-controlled, partially responsive, or unresponsive. On day 14, two patients were well-controlled, and eight partially responded. By the 1st month, four remained partially responsive, and six became unresponsive. At 6 months, three patients were well-controlled, but two showed no clinical improvement. UAS7 scores of the MSC-treated group significantly decreased compared to the control group at 1, 3, and 6 months.
Flow cytometry analysis revealed that on the 14th day, frequencies of CD4+ interferon gamma+ and CD4+ Gata3+ cells were significantly higher in the treated group than in the control group. In addition, there were significant differences in TGF-b1 and IDO values between the treated and control groups, suggesting that these immunological effects might result from transient cytokine changes.[11]
Clinical perspectives on MSCT in CU and AD
The immunologic functions of MSCs imply that MSCT could offer symptomatic, causative, and even preventive treatment benefits. In a clinical trial for AD, allogeneic MSCs were well tolerated without rejection.
Animal studies revealed that systemically administered MSCs through intravenous injection tend to localize in the lungs and show positive effects in CSU, indicating systemic action. Similarly, in AD, subcutaneous administration of MSCs resulted in local and systemic improvements.
MSCT has shown efficacy in both in vitro and in vivo animal studies, leading to successful predictions and outcomes in human trials. Although human diseases and animal models differ, the promising results from animal studies suggest that future human clinical trials are likely to be successful.
MSCs can be administered subcutaneously or intravenously. Both methods have been effective, but subcutaneous injection is considered safer due to the risk of pulmonary embolism associated with intravenous injection. Despite intravenous administration showing higher efficacy in animal models of AD, subcutaneous administration was preferred for subsequent human trials for safety reasons.
In the limited clinical trials conducted for AD and CSU, the effective MSC dose was approximately 5 × 107 cells. In CSU, two injections 2 weeks apart proved successful. Both studies demonstrated that MSCT was effective and safe, with no severe adverse effects.
Notably, in a human study on MSCT for CSU, clinical scores improved and remained stable for 6 months in patients treated with MSCs, in contrast to recurrence in those treated with omalizumab, a new and effective biologic for CSU. These findings indicate that MSCs hold significant potential as a novel therapeutic approach. [10,12]
Autoimmune disorders
Autoimmune bullous disorders
Pemphigus
Although corticosteroids and other immunosuppressants are still the first-line treatment for pemphigus, some patients are still resistant to medication, necessitating the investigation of alternative treatments. According to the postulated mechanism of action, the immune system is repopulated by the transplanted SCs, and the number of autoreactive immune cells decreases, which reestablishes the immunological equilibrium. Case studies and series have been published from India on the use of autologous and allogeneic hematopoietic SCs for the successful treatment of resistant pemphigus. The most frequent adverse effect noted was infection, eventually leading to sepsis and death.[13-16] Table 3 summarizes the details of a few studies on SC-based therapy in pemphigus patients.
| Type of study with reference | Inclusion criteria | Results | Type of stem-cell treatment used | Significant side effects |
|---|---|---|---|---|
| Case series[16] |
|
Autologous peripheral HSCT | In 10/11, 9/11, and 6/8 patients, complete remission was attained and maintained at 6 months, 1 year, and 5 years. 5 and 6 months after transplant, 2 patients experienced relapses. | Fever, headache, deranged liver function, infection |
| Case series[15] |
|
Cytokine-stimulated allogeneic HSCT | Within 24 h of HSCT, recovery started, and after 6 months, new lesions ceased appearing. Throughout an average follow-up of 8.02 years, every patient remained healthy and had no new lesions or recurrences. | No significant adverse effects |
| Case report[14] |
|
Allogeneic HSCT Conditioning regimen: Alemtuzumab Adjuvant: Oral sirolimus |
Severity reduced on 9 months post-transplant | Arthralgia |
HSCT: Hematopoietic stem-cell transplantation
Epidermolysis bullosa (EB)
SC treatments are being tested in uncommon genetic blistering illnesses such as recessive dystrophic EB (RDEB), which cause serious disease consequences such as mitten abnormalities and aggressive epithelial malignancies. Intravenous therapy or MSC injections into chronic wounds are novel techniques for epithelial regeneration. According to preliminary research, in DEB mice models, intradermal injections of human BM-MSCs enhanced dermal-epidermal integrity and repaired immature anchoring fibrils.[17] Similar preclinical findings were described by Conget et al., wherein type VII collagen was replenished at the dermoepidermal interface following intradermal BM-MSC injection from healthy donors into two chronic wounds. The administration reduced blister formation and led to the re-epithelialization of chronic ulcers. Furthermore, tissue-regenerating cytokines may trigger self-healing mechanisms in RDEB skin. Later investigations had doubts about the role of SC therapy in phenotypic improvement.[18] A study found that a single intradermal injection of allogeneic fibroblasts enhanced wound healing in RDEB patients for 28 days, although this effect faded afterward.[19] In a different study, type VII collagen expression and wound healing in chronic non-healing ulcers of RDEB patients were enhanced by both allogeneic cultured fibroblasts in suspension solution and suspension solution alone, independent of type VII collagen regeneration.[20] Therefore, it was hypothesized that the mechanical stimulation of intradermal injections would enhance wound healing by upregulating the expression of heparin binding-endothelial growth factor-like growth factor in response to subclinical inflammations following skin injections.[21]
Systemic (intravenous) allogeneic BM-MSCs enhanced wound healing and reduced skin redness, quality of life, and tolerability in ten children of RDEB. Given that skin biopsies taken 2 months following therapy revealed no increase in type VII collagen or new anchoring fibrils, it is possible that the immune system’s inhibition and regulation was the cause of this clinical improvement. In another clinical trial, BM-MSCs with or without cyclosporine reduced blistering and healing time. After therapy, electron microscopy showed more anchoring fibrils in this study.[18] However, future clinical trials must determine allogeneic MSC application methods and appropriate dosage.
Bone marrow transplantation (BMT) has also been studied in severe generalized junctional EB. However, keratinocytes generate laminin-332, not fibroblasts. Thus, it is unclear if rectified donor BM-derived cells in the dermis can restore basement membrane protein without epithelial cell correction. It was previously thought that keratinocytes differentiated from BM-derived MSCs. Laminin-332 was also generated by hematopoietic and MSCs originating from BM. According to certain clinical investigations, BMT increases the expression of laminin-332 at the dermoepidermal junction. BM-derived SCs may target additional epithelial-synthesized proteins implicated in severe forms of EB.[18,19]
Psoriasis
Although there has been significant progress in recent years in understanding the etiology and pathogenesis of psoriasis, it is still not entirely clear. At present, interest has been focused on the notion that specific forms of SC malfunction may be a factor contributing to the dysregulation of the inflammatory response in psoriasis.[22]
The inspiration came from observing psoriasis patients who were successfully treated with hematopoietic SC therapy go into long-term remission. On the other hand, instances of acquired psoriasis following BMT from donors who used to have the condition have also been documented. This infers that hematopoietic SCs play a major role in the development of illness. MSCs have also been successfully used in a small number of trials. MSC engraftment, as well as its immunomodulatory actions, may be responsible for clinical improvements. However, SC transplantation is not a popular choice of treatment for psoriasis due to the availability of more affordable and secure alternatives.[23]
Vitiligo
Vitiligo is an acquired condition presenting as depigmented patches due to the absence of melanocytes. It has been demonstrated that cell-based therapy, such as skin grafting and cell transplantation, helps regain pigment. Phosphatase and tensin homolog (PTEN) overexpression may contribute to melanocyte dysfunction in vitiligo, and suppression of the PTEN/PI3K/AKT pathway contributes to the therapeutic benefits of MSCs. In addition, it has been demonstrated that adipose tissue-based stem cells (ADSCs) may serve as a source of growth factors for melanocytes. In an animal model, grafting melanocytes with the inclusion of ADSCs improved treatment efficacy in comparison to graft containing only melanocytes. Transplantation with keratinocytes, melanocytes, or a combination of both is another quick and secure technique to treat vitiligo, which has been shown to result in adequate re-pigmentation in humans. However, SC therapy is only likely to be effective for those who have segmental and localized vitiligo.[24,25]
Systemic sclerosis (SS)
SS is one of the first autoimmune disorders where SC therapy was used for disease modification. It was non-specifically immunoablates aberrant self-reactive T- and B-cells reestablishing a tolerant immune system. Autologous hematopoietic SC therapy has decreased treatment-related mortality.[26] Furthermore, there are no chances of GvHD. SC therapy for SS was evaluated in three randomized controlled trials with positive results: the American Scleroderma SC versus Immune Suppression Trial (phase 2, 19 patients), the Autologous SC Transplantation International Scleroderma Trial (phase 3, 156 patients), and the Scleroderma Cyclophosphamide or Transplantation study (phase 3, 75 patients). Individuals with pulmonary, cardiac, or renal involvement were excluded from all three trials because serious comorbidities are absolute contraindications for hematopoietic SC therapy.[27-29] It is been shown to work better than traditional immunosuppressive treatments. It is the only disease-modifying approach currently available for preventing organ deterioration and improving skin and pulmonary function, thereby enhancing patients’ overall quality of life. Patients with an acute, rapidly progressing illness and relatively lesser organ damage typically experience better outcomes. Even though some studies claimed that symptoms improved after receiving allogeneic HSC treatment, the overall data on allogeneic HSC effectiveness is still not strong, maybe due to its chances of adverse reactions such as GvHD and opportunistic infections. Hence, careful selection of patients is highly recommended.[30] The details of a few recent studies on SC therapy in SS are shown in Table 4.[29-33]
| Type of study with reference | Inclusion criteria | Methods | Results | Side effects |
|---|---|---|---|---|
| Case series[26] | Total 4 patients were included. Diffuse SS with mRSS of 15 and 1 internal organ involvement. |
Autologous HSCT mobilization: cyclophosphamide and G-CSF Conditioning regimen: cyclophosphamide plus fludarabine plus anti-thymocyte globulin. Outcome measures used are mRSS, PFT. | After 4 years of follow-up, the mean mRSS dropped from 24.5 at baseline to 18.5. The mean FVC rose to 78.5% after a 4-year follow-up, from 65%. |
Nothing significant |
| Total 14 patients Long-term follow-up in a phase II Trial[32] | Interstitial lung disease, refractory digital ulcer, or SS individuals with a disease duration of<3 years and mRSS) ≥15. | Following cyclophosphamide conditioning, HSCT was carried out. A median follow-up of 137 months was observed. | 93% of people survived overall. Within 6 months following HSCT, 8 patients (57%) saw a drop in mRSS of more than 50% from baseline. | 6 patients (43%), experienced side effects. 2 individuals had severe cardiomyopathy; one of them eventually succumbed. |
| Retrospective study, 18 patients[29] | Diffuse SS with rapid progression and a protracted illness. | Autologous HSCT Cyclophosphamide with filgrastim mobilization Exercise routine: cyclophosphamide Outcome measures: 60-month follow-up for mRSS, DLCO, and disease activity using the ESSG scoring system. | mRSS and DLCO in the treatment group were statistically significantly lower than in the control group at 1 year and remained lower at the conclusion of the follow-up. | At 1 year and until the end of the follow-up, mRSS and DLCO in the treatment group were statistically substantially lower than in the control group. |
G-CSF: Granulocyte colony-stimulating factor, HSCT: Hematopoietic stem-cell transplantation, SS: Systemic sclerosis, mRSS: Modified Rodnan skin score, PFT: Pulmonary function test, FVC: Forced vital capacity, ESSG: European schleroderma study group index, DLCO: Diffusion capacity of lung for CO (carbonmonoxide)
SC therapy in morphea
Localized scleroderma, or morphea, is a rare autoimmune disease characterized by thickening and hardening of the skin and underlying tissues due to excessive collagen deposition. Although the precise origin of morphea remains uncertain, an aberrant immune response is thought to be involved. With promising outcomes, numerous researches have looked at the application of MSCs in the management of morphea. Adipose-derived SCs (ADSCs) were used to treat a patient with refractory morphea, and the patient demonstrated notable improvements in skin thickness and mobility after treatment. In a different trial, morphea was treated with bone marrow-derived MSCs combined with phototherapy, which reduced skin lesions and improved skin texture. Treatment for two patients with progressive and resistant scleroderma involved a combination immunotherapy regimen. The course of treatment included intravenous umbilical cord-derived allogeneic MSCs, rituximab, and plasmapheresis. For more than a year, both patients’ symptoms and objective measurements improved. When their symptoms returned, allogeneic MSCs alone were used to treat them, and this had a very positive outcome. Given that the combined therapy was both well-tolerated and efficacious, further extensive research in individuals with progressive, resistant scleroderma may be necessary.[21]
Systemic lupus erythematosus (SLE)
There has been considerable research on MSCs for their therapeutic potential in treating autoimmune disorders, including SLE. Their major role is in maintaining the balance between Th1 and Th2 immune systems. By decreasing the autoantibody production, they reduce the disease activity. Furthermore, there is a significant improvement in renal function, and hence, it is an ideal new treatment option for SLE. [33] Allogeneic BM-MSC transplantation for refractory active SLE patients was first performed by Sun et al. in 2007. Four glucocorticoid treatment-refractory SLE patients had allogeneic MSCT and achieved 12–18 months of disease remission with reduced disease activity, proteinuria, and serum autoimmune antibodies. In addition, peripheral blood CD4+ Foxp3+ regulatory T-cell count increased considerably. [32,33] Subsequently, Wang et al. recruited 40 active SLE patients for multicenter clinical research. Each patient received 106/kg MSCs intravenously twice a week. After 12 months, there were six cases of non-transplant-related adverse events. It included three deaths and three infections. The clinical response rate was 60%, while the overall survival rate was 92.5%. All clinical parameters improved, such as a reduction in 24-hour proteinuria, serum levels of blood urea nitrogen and creatinine, and an increase in serum complement and albumin.[34]
There is a decline in HSC activity in SLE. According to Westerweel et al., SLE patients had lower concentrations of endothelial progenitor cells and circulating HSCs, which made HSC apoptosis worse. Since progenitor cell-mediated endogenous vascular repair is absent in SLE patients, there is an increased risk of atherosclerosis.[35] European Blood and Marrow Transplant and the European League Against Rheumatism registry conducted a retrospective study that revealed that 53 SLE patients from 23 centers had received hematopoietic stem-cell transplantation (HSCT) in the past 6 months. After treatment, 66% of HSCT patients were in remission, and 32% relapsed. Long-term immunosuppressive medication might be able to minimize relapse.[36] In 2007, Loh et al. retrospectively analyzed SLE patients getting auto-HSCT for substantial cardiac involvement and its effects. A total of 13 of 55 study participants had abnormal cardiac results before HSCT. The patients with reduced cardiac function stabilized or improved. No transplant-related or cardiac deaths occurred during follow-up. [37]
Although HSCT is curative with good efficacy, the incidence of adverse effects is significant. Furthermore, it is costly with a high recurrence rate. As a result, its clinical application is rather restricted. However, starting in 2007, Sun et al. successfully performed allogeneic BM-MSCT for the 1st time in the management of refractory SLE. The long-term follow-up effectiveness rate in the clinical investigation of SLE patients was 60%, with no overt adverse effects.[38] The comparison of MSC and HSCT in SLE is shown in Table 5.[39]
| Parameter | HSCT | MSCT |
|---|---|---|
| Therapeutic effect | The relapse rate is nearly 1/3rdwhile some SLE patients achieve remission | Following multi-organ dysfunctions, such as lupus nephritis, MSCT-induced remission was seen in more than half of SLE patients, both in terms of complete and partial clinical remission. |
| Mechanism | During HSCT, high-dose immunosuppression would get rid of autoreactive cells. Both the pathogenic T cell responses against autoantigens and the amount of regulatory T cell populations fluctuate. | Systemic immunoregulatory effects on T cells, B cells, plasma cells, dendritic cells, and macrophages, among other immune regulatory cells. |
| Adverse effects | Heart failure, secondary AD, allergies, elevated liver enzymes, bone pain, and infection (CMV or bacterial/fungal). | Mild adverse effects including light-headedness and warmth are experienced by a very tiny percentage of people. |
| Cost | Comparatively expensive when it comes to high-dose immunosuppressive medications and complex cell conditioning. | In comparison to HSCs, its cost is significantly cheaper and it offers benefits in terms of patient acceptance. |
HSCT: Hematopoietic stem-cell transplantation, MSCT: Mesenchymal stem-cell therapy, SLE: Systemic lupus erythematosus, CMV: Cytomegalovirus, AD: Atopic dermatitis
SC therapy for esthetic indications
Skin rejuvenation
SCs are used for the remodeling of skin after promising preclinical findings. Subcutaneously, injecting ASCs into mice with UVB-induced wrinkles improved wrinkles and increased skin thickness and collagen content. Epidermal penetration has been facilitated by the combination of SCs with microneedling. In two randomized, controlled, and blinded split-facial studies, one-half of the face received microneedling, and the other half received SC-conditioned medium (CM). Compared to baseline and placebo, therapy reduced wrinkles, erythema pigmentation, and pore size and improved overall patient satisfaction.[40] Laser resurfacing has been combined with SC treatment. Following fractional carbon dioxide laser resurfacing, ASC-CM was administered to half of the face, and the other half received a placebo in the form of Dulbecco’s Modified Eagle’s Medium (DMEM) free of fetal bovine serum (FBS). ASC-CM treatment of the experimental half of the face improved patient satisfaction and all objective clinical assessment scores, such as pigmentation, hydration, and skin roughness, compared to baseline and placebo after three sessions. At 21 days post-procedure, histology showed enhanced skin collagen and elastin content on the treatment side compared to placebo. [41] Autologous fat transfer procedures, which are performed after liposuction, are convenient and popular due to their advantage of volume loss reversal. Due to SCs in fat grafts, they have positive effects on skin regeneration, such as a reduction in wrinkles, pores, and pigmentation. [42]
Fat transfer can be either macrofat (conventional utilizing large multiport cannulas), microfat, or nanofat (emulsified and filtered into liquid suspension). Given the final solution contents and viscosity, macrofat is employed for lipofilling major defects. Because nanofat does not contain live adipocytes, it is mostly employed for skin regeneration, whereas microfat is used for more delicate areas. [43]
Studies on SC therapy for skin rejuvenation are shown in Table 6. [40,44-46]
| Number of patients | Details of the study and procedure | Results |
|---|---|---|
| 15 Females[40] | Every 4 weeks for 3 sessions, half of the face was randomly assigned to receive treatment with microneedling plus stem-cell conditioned media, while the other half received only microneedling. | At 4 weeks into the treatment, there was a significant improvement in the physician’s global assessment, patient satisfaction scores, fine wrinkles, and dermal collagen on the treatment side compared to the baseline and placebo. |
| 48 Females[44] | Received regular saline or a medium conditioned by amniotic membrane SCs in addition to microneedling to the face every 2 weeks for 3 sessions. | At 8 weeks, there were notable improvements in clinical measurements of pores, wrinkles, spot-polarized, and spot-UV characteristics when compared to placebo. |
| 1 Male and 5 Female patients[45] | After liposuction, under local anesthetic, received preauricular injections of either expanded MSCs or autologous fat and SVF. | Histologic examination revealed that both treatment groups had decreased reticular cutaneous elastosis and more hydration compared to baseline. |
| 48 Male and 2 Female patients[48] | PRP and nanofat suspensions injected into the face once using a fanning technique. | Texture, elasticity, shine, firmness, fine wrinkles, and skin hydration were all reported improved in all patients. |
SC: Stem cell, PRP: Platelet-rich plasma, UV: Ultraviolet, MSCs: Mesenchymal stem cells, SVF: Stromal vascular fraction
Role of SCs in cosmeceuticals
The utility of SCs in cosmetology is unclear. Hydrophilic compounds beyond 500 daltons cannot permeate intact stratum corneum. Topical formulations containing SCs with a larger molecular weight and their growth factors can enter both the epidermis and dermis, notwithstanding this limitation. The bulk of cosmeceutical SCs are also produced from plant sources, which cannot mimic human SCs and are not long-lasting. According to in vitro research, the application of the SCs increased the cellular proliferation of human SCs in a concentration-dependent manner. In a second in vitro experiment, they discovered that when the plant SCs were stressed with ultraviolet radiation, their vitality increased.[47] Numerous other plants have been investigated, such as edelweiss, ginger, and tomato vines (Lycopersicon esculentum), among others. However, in-depth clinical trials are still lacking. These have demonstrated encouraging outcomes in terms of preventing oxidative stress on the human SCs that are now in existence, reducing inflammation, and scavenging free radicals. A vehicle-controlled, multicenter, and double-blind study was conducted using preparations of a- and b-defensin. A total of 44 female patients were randomized to receive either a placebo or the entire recipe, which included a cream, mask, and serum containing a- and b-defensins. These items were administered twice daily. Epidermal thickness increased significantly at 12 weeks on histology. Appearance of pores and superficial wrinkles decreased with the overall improvement in skin tone and evenness.[48]
Androgenetic alopecia (AGA)
A commercialized adipose-derived SC-CM (ADSC) containing lyophilized proteins is cultivated from ASCs of healthy adult women. In a study, ASC-CM was injected intradermally into AGA patients’ scalps every 3–5 weeks for 4–6 months for a total of six sessions. Initial investigations showed subjective improvement in terms of major visual analog scales and patient satisfaction. Trichograms taken 1–3 months after the last treatment revealed significant hair growth over the baseline. In a different trial, saline was injected into half of the scalp and ASC-CM into the other. Compared to the untreated half, the trichogram’s hair counts were much greater. In a different experiment, commercial ASC-CM was used for 12 weekly AGA therapy sessions along with a microneedle roller. Hair density and thickness increased significantly at the end of 12 weeks in terms of trichogram imaging results.[49]
A study evaluated the role of SVF in AGA. A pure fat graft and SVF were prepared from tumescent liposuction lipoaspirate and injected subcutaneously into the scalp. Six patients reached the 24-week objective improvement scores when hair counts increased significantly compared to baseline. However, anagen, telogen hair count, and thickness changes were not statistically significant. Treatment of hair loss has been explored from other SC sources.[50] Another study used scalp punch biopsies to mechanically disintegrate and centrifuge autologous SCs from hair follicles. Microscopy showed dermal papilla CD44+ SCs and bulge with CD200+ SCs. After that, 11 AGA patients had two intradermal injections of this suspension of SCs, separated by 60 days, which after 23 weeks enhanced both the number and density of hair compared to the baseline and placebo. These results were validated by another clinical research.[51]
SC therapy for wound healing
Since approximately 50% of serious skin wounds fail to heal after being treated, they are an increasing problem. Making use of SCs is important, particularly in wounds that are challenging to cure, such as lesions caused by diabetes, severe injury, vascular dysfunction, and extensive burns. Several internal and external elements are involved in the intricate process of wound healing. Chronic wounds result from a disruption in one of the phases of healing, which lengthens inflammation. By releasing various growth factors, including vascular endothelial growth factor, insulin-like growth factor, hepatocyte growth factor, and fibroblast growth factor 2, ADSCs are thought to aid in the healing of wounds indirectly. Each of these contributes to the anti-inflammatory, anti-oxidative, and anti-apoptotic properties.[52] In prior studies, patients with chronic non-healing wounds received tissue-engineered skin equivalents such as human cultured dermis, allogeneic and autologous fibroblasts, or keratinocytes. Moderate to complete wound healing was observed several weeks following treatment. Similar results are also seen in cases of burn injury. However, following treatment with skin substitutes, different tissue is produced that lacks adnexal characteristics, such as hair follicles, melanocytes, and sweat glands.[53]
Exosome-based SC therapy for wound healing
Exosome derived from SC (EdSC) is an innovative method of enhancing the wound-healing process. The smallest SC extracellular vesicle, EdSC, has a lipid bilayer structure with a diameter of 30–150 nm. EdSC has been shown to regulate inflammatory cells, activate keratinocytes, fibroblasts, and endothelial cells, and alter collagen I and III ratios during wound healing. Injecting EdSC intravenously is the method of administration used most frequently. For instance, Hu et al. found that injecting EdSC directly into a mouse wound site can enhance the fibroblasts’ activity and hasten wound healing. EdSC can also be administered subcutaneously to promote wound healing. Furthermore, subcutaneously administered melatonin stimulated EdSCs improved diabetic wound healing by controlling the polarization of macrophages.[54]
Although injection as a process is straightforward and effective, its rapid clearance rate limits EdSC therapeutic activity. In recent years, numerous studies have paired EdSC with hydrogel to extend its efficacy and durability to expedite wound healing. Hydrogels can absorb a lot of EdSC-containing solution and increase wound hydration when applied to the wound bed. It helps loaded cells repair faster by maintaining a favorable wound bed microenvironment.[55]
Cutaneous malignancies
Melanoma
Even with oncogene-directed therapy and immunotherapy, melanoma is an aggressive, chemo- and radio-resistant malignancy. Recently, it has been proposed that tumor SCs, which are a tiny population of tumor-initiating cells, promote carcinogenesis. Melanoma SCs have been considered for this notion, originally developed for human myeloid leukemia. Self-renewing tumor SCs can proliferate indefinitely, reject numerous therapies, and cause tumor relapse. Thus, future medicines can target biomarkers, microenvironments, and melanoma progenitor cells.[56] Melanoma SCs are positive for CD133, CD271, and aldehyde dehydrogenase. In clinical trials, rituximab has regressed chemotherapy-refractory melanoma because its SCs express CD20. A monoclonal antibody targeting ABCB5+ melanoma SCs inhibited tumors in mice. Since mutant B-RAF activates the mitogen-activated protein kinase (MAPK) signaling pathway to drive melanoma tumor proliferation and B-RAF inhibitors can cause MAPK pathway reactivation through a pathway known as an “escape route,” MAPK signaling molecules may be promising targets to overcome melanoma resistance. Inhibiting critical SC factors or administering differentiation factors reduces tumor SC tumorigenicity.[57,58]
Merkel cell carcinoma
Metastatic treatment for this rare cutaneous tumor is unknown. In recent years, the Merkel cell polyomavirus as the causal agent has been identified and understood. It demonstrates that transitory or resident polyomaviruses capable of neoplastic transformation are present in healthy human skin. Positive for polyomavirus Merkel cell carcinomas are distinct from polyomavirus-negative malignancies in every way, including morphology, gene expression, signaling pathways, microRNA profiles, dysregulated immune surveillance, and post-translational modifications. This affects the prognosis. Recent studies imply that polyomavirus-positive and negative Merkel cell carcinomas originate from dermal and epidermal SCs, respectively. Research on Merkel cell carcinoma SCs may help create targeted therapies. Studies combining polychemotherapy with autologous peripheral blood SC transplantation produced improvement in terms of a 6-month remission.[59,60]
USE OF ARTIFICIAL INTELLIGENCE (AI) IN iPSCS
Due to the enormous volume of data analysis, rising quantity and complexity, lack of standardizing techniques, human error, and extremely difficult data administration, the traditional approach to regenerative medicine and cell-based therapies faces several challenges. This increases the difficulty and chance of inaccuracy in the process of using decision-making procedures and developing conclusions. The inclusion of iPSCs in different experimental and therapeutic procedures requires the identification of iPSC-derived cells, a thorough evaluation of their quality, and characterization of the cell type. Large-scale cultures cannot afford the time-consuming and are prone to mistakes in the process of manually evaluating colony morphology. To circumvent this limitation, multiple research groups have implemented diverse AI algorithms to establish an automated process for accurate segmentation and assessment of colony quality.[61,62] An automated technique for identifying iPSC colony photographs with a resolution of 1608*1208 was the subject of a study by Joutsijoki et al. utilizing ML classifiers, namely, support vector machines and k-Nearest Neighbors (k-NN). Scale-invariant feature transform descriptors were also employed for extracting features. The Euclidean measure and equal weighting of the k-NN classifier generated the greatest results, with an accuracy of 62.4%, which was measured in contrast to past studies.[63]
STATUS OF SC THERAPY IN INDIA
The 2017 National Guidelines for SC Research, published by the Department of Biotechnology (DBT) and the Indian Council of Medical Research (ICMR), offer the fundamental regulations for SC research in India. These regulations list the different ethical concerns, screening, research classification, levels of SC manipulation, manufacture and release standards for SCs, banking, therapeutic uses, publicity, and advertisements. According to the regulations, The commercial use of SCs as therapeutic components is prohibited. It must be understood that no human SC administration outside of clinical studies is permitted. According to the National Guidelines created by the ICMR and DBT, only hematopoietic SC therapy has been approved in India. As an appendix, there is a list of every center where it is performed.[64,65] Hematopoietic SC treatment is authorized by the American Society for Blood and Marrow Transplantation (ASBMT) for around 31 adult disorders and 43 pediatric diseases. Among the indications include solid tumors, hematological malignancies, and non-malignant conditions such as juvenile rheumatoid arthritis, dyskeratosis congenita, aplastic anemia, and Fanconi’s anemia. The Task Force of ASBMT had approved the use of hematopoietic SC therapy in children (18 years of age) but not in adults in the case of SS, one of the dermatological indications.[66]
SIDE EFFECTS AND WORKING DIFFICULTIES
Manufacturing and contamination issues
The success of therapy depends on maintaining the consistency of SC manufacturing methods. Formal safety evaluations and thorough preclinical testing are required. It is imperative to mitigate contamination concerns and thoroughly characterize the cells before introducing them into the body. It can be difficult to maintain the genetic and phenotypic behavior of the cells during long-term culture because excessive transit can result in genetic abnormalities.[67]
Post-transplant SC distribution
It is essential to track the SCs’ distribution throughout the host after transplantation to make sure they localize correctly. Since pluripotent SCs can develop into teratomas, it is critical to keep an eye on their activities to avoid the development of tumors or ectopic tissue. Methods such as green fluorescent protein (GFP) labeling and quantitative polymerase chain reaction, nuclear magnetic resonance, or magnetic resonance imaging scanning can be used to follow the distribution and behavior of these cells.[68]
Challenges in developing nations
Since SC treatments can be costly, many people in developing countries cannot afford them. Furthermore, these nations might not have the infrastructure and trained labor required for SC research and therapy. Government assistance is lacking, which impedes progress even further. Funding from the commercial sector, international partnerships, and the encouragement of exchange studies could all help overcome these obstacles and make SC therapy research and adoption in developing countries easier.
CHALLENGES AND FUTURE DIRECTIONS
It is very important that a new product being tested on humans is safe. One of the most recent therapeutic items in medicine, stem-cell-based therapies, is challenging to bring to market since a lot of factors need to be considered. Risks associated with stem-cell-based therapies include immunological reactivity, SC migration to unsuitable locations, genetic instability during long-term expansion, and others. All obstacles depend on the type of SC, indication for use, mode of delivery, and many other aspects. Clinical trial approval from a competent regulatory authority requires different tests for each study phase and does not generalize study outcomes. The Food and Drug Administration uses in vitro and in vivo preclinical studies to control stem-cell-based products. Another problem is the long length of a clinical trial before the product is introduced to the market for use.[69]
An attractive future option for regenerative medicine is the use of cell derivatives, such as exosomes, Wharton’s jelly, amniotic fluid, and others, to treat diseases. Recently, preclinical studies have evaluated and optimized these products’ safety and efficacy. Due to promising results from preclinical research and anticipated commercial benefits, the market for regenerative medicine is growing, and rivalry among manufacturers working to generate cell products has intensified. We can thus be more optimistic about the future of SC-based therapies due to the significant investments made in the development of the regenerative medicine sector in recent years by government agencies, academic institutions, and private groups.[70,71]
CONCLUSION
SCs are progenitor cells that can develop into a variety of adult cell types. They assist in preserving healthy skin homeostasis. When SCs interact with damaged skin, they produce growth factors along with the reduction of proinflammatory mediators, the control of the immune system, the prevention of oxidative stress, and the encouragement of both angiogenesis and cell growth. Studies on alopecia, skin rejuvenation, segmental vitiligo, and wound healing have produced good to extraordinary results with few side effects. However, due to the complexity of these disorders, SS, pemphigus, and EB had poor to intermediate outcomes and a high frequency of significant adverse effects, which were more likely to recur. More research is required to assess their effectiveness and any potential risk-benefit ratio on a case-specific basis. SC therapy offers a potentially beneficial therapeutic option for a variety of dermatologic disorders for which current medical therapies do not offer a sufficient cure.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
Patient’s consent was not required as there are no patients in this study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship
Nil
References
- Intravenous infusion of bone marrow in patients receiving radiation and chemotherapy. N Engl J Med. 1957;257:491-6.
- [CrossRef] [PubMed] [Google Scholar]
- The Nobel prize in physiology or medicine. 2007. Available from: http://nobelprize.org/nobel_prizes/medicine/laureates/2007/index.html [Last accessed on 2007 Oct 08]
- [Google Scholar]
- Epidermal stem cells of the skin. Annu Rev Cell Dev Biol. 2006;22:339-73.
- [CrossRef] [PubMed] [Google Scholar]
- Generation and characterization of multipotent stem cells from established dermal cultures. PLoS One. 2012;7:e50742.
- [CrossRef] [PubMed] [Google Scholar]
- Induced pluripotent stem cells in research and therapy. Malays J Pathol. 2012;34:1-13.
- [Google Scholar]
- Concise review: Role of mesenchymal stem cells in wound repair. Stem Cells Transl Med. 2012;1:142-9.
- [CrossRef] [PubMed] [Google Scholar]
- Stem cell therapy in dermatology. Indian J Dermatol Venereol Leprol. 2021;87:753-67.
- [CrossRef] [PubMed] [Google Scholar]
- T helper (Th)1, Th17 and Th2 imbalance in mesenchymal stem cells of adult patients with atopic dermatitis: At the origin of the problem. Br J Dermatol. 2017;176:1569-76.
- [CrossRef] [PubMed] [Google Scholar]
- Disease-specific primed human adult stem cells effectively ameliorate experimental atopic dermatitis in mice. Theranostics. 2019;9:3608-21.
- [CrossRef] [PubMed] [Google Scholar]
- Mesenchymal stem cells: A potential treatment approach for refractory chronic spontaneous urticaria. Stem Cell Rev Rep. 2021;17:911-22.
- [CrossRef] [PubMed] [Google Scholar]
- The diagnosis and management of acute and chronic urticaria: 2014 update. J Allergy Clin Immunol. 2014;133:1270-7.
- [CrossRef] [PubMed] [Google Scholar]
- Clinical trial of human umbilical cord blood-derived stem cells for the treatment of moderate-tosevere atopic dermatitis: Phase I/IIa studies. Stem Cells. 2017;35:248-55.
- [CrossRef] [PubMed] [Google Scholar]
- High-dose immune suppression and autologous hematopoietic stem cell transplantation in refractory pemphigus foliaceus. Bone Marrow Transplant. 2004;34:1097-8.
- [CrossRef] [PubMed] [Google Scholar]
- Pemphigus vulgaris treated with allogeneic hematopoietic stem cell transplantation following non-myeloablative conditioning. Eur Rev Med Pharmacol Sci. 2010;14:785-8.
- [Google Scholar]
- Allogenic hematopoietic stem cell transplantation in pemphigus vulgaris: A single-center experience. Indian J Dermatol. 2012;57:9-11.
- [CrossRef] [PubMed] [Google Scholar]
- Application of autologous hematopoietic stem cell transplantation for pemphigus. Int J Dermatol. 2017;56:296-301.
- [CrossRef] [PubMed] [Google Scholar]
- High local concentrations of intradermal MSCs restore skin integrity and facilitate wound healing in dystrophic epidermolysis bullosa. Mol Ther. 2015;23:1368-79.
- [CrossRef] [PubMed] [Google Scholar]
- Replenishment of type VII collagen and re-epithelialization of chronically ulcerated skin after intradermal administration of allogeneic mesenchymal stromal cells in two patients with recessive dystrophic epidermolysis bullosa. Cytotherapy. 2010;12:429-31.
- [CrossRef] [PubMed] [Google Scholar]
- Fibroblast cell therapy enhances initial healing in recessive dystrophic epidermolysis bullosa wounds: Results of a randomized, vehicle-controlled trial. Br J Dermatol. 2013;169:1025-33.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of dystrophic epidermolysis bullosa with bone marrow non-hematopoeitic stem cells: A randomized controlled trial. Dermatol Ther. 2016;29:96-100.
- [CrossRef] [PubMed] [Google Scholar]
- Cell therapy in dermatology. Cold Spring Harb Perspect Med. 2014;4:a015156.
- [CrossRef] [PubMed] [Google Scholar]
- Mesenchymal stem cells for the treatment of psoriasis: A comprehensive review. Clin Exp Dermatol. 2020;45:824-30.
- [CrossRef] [PubMed] [Google Scholar]
- Transmission of psoriasis by allogeneic bone marrow transplantation and blood transfusion. Blood Cancer J. 2015;5:e288.
- [CrossRef] [PubMed] [Google Scholar]
- Mesenchymal stem cells promote human melanocytes proliferation and resistance to apoptosis through PTEN pathway in vitiligo. Stem Cell Res Ther. 2020;11:26.
- [CrossRef] [PubMed] [Google Scholar]
- Treatment of vitiligo with autologous cultured keratinocytes in 27 cases. Eur J Plast Surg. 2013;36:651-6.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous non-myeloablative hematopoietic stem cell transplantation in patients with systemic sclerosis. Bone Marrow Transplant. 2007;40:549-55.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous hematopoietic stem cell transplantation vs. intravenous pulse cyclophosphamide in diffuse cutaneous systemic sclerosis: A randomized clinical trial. JAMA. 2014;311:2490-8.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous non-myeloablative haemopoietic stem-cell transplantation compared with pulse cyclophosphamide once per month for systemic sclerosis (ASSIST): An open-label, randomised phase 2 trial. Lancet. 2011;378:498-506.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous hematopoietic stem cell transplantation has better outcomes than conventional therapies in patients with rapidly progressive systemic sclerosis. Bone Marrow Transplant. 2017;52:53-8.
- [CrossRef] [PubMed] [Google Scholar]
- Transplantation for autoimmune diseases in North and South America: A report of the Center for International Blood and Marrow Transplant Research. Biol Blood Marrow Transplant. 2012;18:1471-8.
- [CrossRef] [PubMed] [Google Scholar]
- Stem cell transplant in systemic sclerosis: An Indian experience. Int J Rheum Dis. 2018;21:859-65.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous hematopoietic stem cell transplantation for Japanese patients with systemic sclerosis: Long-term follow-up on a phase II trial and treatment-related fatal cardiomyopathy. Mod Rheumatol. 2018;28:879-84.
- [CrossRef] [PubMed] [Google Scholar]
- Abnormality of bone marrow-derived stem cells in patients with systemic lupus erythematosus. Lupus. 2007;16:121-8.
- [CrossRef] [PubMed] [Google Scholar]
- Umbilical cord mesenchymal stem cell transplantation in active and refractory systemic lupus erythematosus: A multicenter clinical study. Arthritis Res Ther. 2014;16:R79.
- [CrossRef] [PubMed] [Google Scholar]
- Haematopoietic and endothelial progenitor cells are deficient in quiescent systemic lupus erythematosus. Ann Rheum Dis. 2007;66:865-70.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous stem cell transplantation for systemic lupus erythematosus. Lupus. 2004;13:359-65.
- [CrossRef] [Google Scholar]
- Autologous hematopoietic stem cell transplantation in systemic lupus erythematosus patients with cardiac dysfunction: Feasibility and reversibility of ventricular and valvular dysfunction with transplant-induced remission. Bone Marrow Transplant. 2007;40:47-53.
- [CrossRef] [PubMed] [Google Scholar]
- Umbilical cord mesenchymal stem cell transplantation in severe and refractory systemic lupus erythematosus. Arthritis Rheum. 2010;62:2467-75.
- [CrossRef] [PubMed] [Google Scholar]
- Stem cell therapy in lupus. Rheumatol Immunol Res. 2022;3:61-8.
- [CrossRef] [PubMed] [Google Scholar]
- Skin rejuvenation by microneedle fractional radiofrequency and a human stem cell conditioned medium in Asian skin: A randomized controlled investigator blinded split-face study. J Cosmet Laser Ther. 2013;15:25-33.
- [CrossRef] [PubMed] [Google Scholar]
- The efficacy of conditioned media of adipose-derived stem cells combined with ablative carbon dioxide fractional resurfacing for atrophic acne scars and skin rejuvenation. J Cosmet Laser Ther. 2016;18:138-48.
- [CrossRef] [PubMed] [Google Scholar]
- Fat grafting for facial filling and regeneration. Clin Plast Surg. 2015;42:289-300.
- [CrossRef] [PubMed] [Google Scholar]
- Nanofat grafting basic research and clinical applications. Plast Reconstr Surg. 2013;132:1017-26.
- [CrossRef] [PubMed] [Google Scholar]
- The effects of amniotic membrane stem cell-conditioned medium on photoaging. J Dermatol Treat. 2019;30:478-82.
- [CrossRef] [PubMed] [Google Scholar]
- Antiaging treatment of the facial skin by fat graft and adipose-derived stem cells. Plast Reconstr Surg. 2015;135:999-1009.
- [CrossRef] [PubMed] [Google Scholar]
- Subcutaneous injections of nanofat adipose-derived stem cell grafting in facial rejuvenation. Plast Reconstr Surg Glob Open. 2020;8:e2550.
- [CrossRef] [PubMed] [Google Scholar]
- Overview of plant stem cells in cosmeceuticals. Plast Surg Nurs. 2014;34:148-9.
- [CrossRef] [PubMed] [Google Scholar]
- Multi-center, double-blind, vehicle-controlled clinical trial of an alpha and beta defensin-containing anti-aging skin care regimen with clinical, histopathologic, immunohistochemical, photographic, and ultrasound evaluation. J Drugs Dermatol. 2018;17:426-41.
- [Google Scholar]
- Clinical use of conditioned media of adipose tissue-derived stem cells in female pattern hair loss: A retrospective case series study. Int J Dermatol. 2015;54:730-5.
- [CrossRef] [PubMed] [Google Scholar]
- Hair follicle growth by stromal vascular fraction-enhanced adipose transplantation in baldness. Stem Cells Cloning. 2017;10:1-10.
- [CrossRef] [PubMed] [Google Scholar]
- Autologous cellular method using micrografts of human adipose tissue derived follicle stem cells in androgenic alopecia. Int J Mol Sci. 2019;20:3446.
- [CrossRef] [PubMed] [Google Scholar]
- The use of adipose-derived stem cells in selected skin diseases (vitiligo, alopecia, and nonhealing wounds) Stem Cells Int. 2017;2017:4740709.
- [CrossRef] [PubMed] [Google Scholar]
- Current status and future of skin substitutes for chronic wound healing. J Cutan Med Surg. 2017;21:23-30.
- [CrossRef] [PubMed] [Google Scholar]
- Exosomes derived from human adipose mensenchymal stem cells accelerates cutaneous wound healing via optimizing the characteristics of fibroblasts. Sci Rep. 2016;6:32993.
- [CrossRef] [PubMed] [Google Scholar]
- Exosomes derived from human umbilical cord blood mesenchymal stem cells stimulates rejuvenation of human skin. Biochem Biophys Res Commun. 2017;493:1102-8.
- [CrossRef] [PubMed] [Google Scholar]
- Stem cells, melanoma and cancer stem cells: The good, the bad and the evil? G Ital Dermatol Venereol. 2009;144:287-96.
- [Google Scholar]
- Melanoma stem cells: The past, present and future. J Stem Cell Res Ther. 2018;4:89-90.
- [CrossRef] [Google Scholar]
- Identification of cells initiating human melanomas. Nature. 2008;451:345-9.
- [CrossRef] [PubMed] [Google Scholar]
- Are there multiple cells of origin of Merkel cell carcinoma? Oncogene. 2018;37:1409-16.
- [CrossRef] [PubMed] [Google Scholar]
- Viral etiology of merkel cell carcinoma: Implications in diagnosis, prognosis, therapy and prevention. Int J Clin Dermatol Res. 2015;3:1-2.
- [CrossRef] [Google Scholar]
- Prediction of metabolism of drugs using artificial intelligence: How far have we reached? Curr Drug Metab. 2016;17:129-141.
- [CrossRef] [PubMed] [Google Scholar]
- The practical implementation of artificial intelligence technologies in medicine. Nat Med. 2019;25:30-6.
- [CrossRef] [PubMed] [Google Scholar]
- Machine learning approach to automated quality identification of human induced pluripotent stem cell colony images. Comput Math Methods Med. 2016;2016:3091039.
- [CrossRef] [PubMed] [Google Scholar]
- The National guidelines for stem cell research (2017) What academicians need to know? Perspect Clin Res. 2019;10:148-54.
- [CrossRef] [PubMed] [Google Scholar]
- Unproven stem cell therapies in India: Regulatory challenges and proposed paths forward. Cell Stem Cell. 2018;23:649-52.
- [CrossRef] [PubMed] [Google Scholar]
- Indications for autologous and allogeneic hematopoietic cell transplantation: Guidelines from the American society for blood and marrow transplantation. Biol Blood Marrow Transplant. 2015;21:1863-9.
- [CrossRef] [PubMed] [Google Scholar]
- Grand challenges in stem cell treatments. Front Cell Dev Biol. 2013;1:2.
- [CrossRef] [PubMed] [Google Scholar]
- Stem cell therapies in clinical trials: Progress and challenges. Cell Stem Cell. 2015;17:11-22.
- [CrossRef] [PubMed] [Google Scholar]
- Stem cell therapy: From idea to clinical practice. Int J Mol Sci. 2022;23:2850.
- [CrossRef] [PubMed] [Google Scholar]
- Stem cells in aesthetic dermatology: Bioethical and professional obligations. Arch Dermatol Res. 2019;311:833-5.
- [CrossRef] [PubMed] [Google Scholar]
- Stem Cells as a therapeutic choice in dermatological disorders. Curr Stem Cell Res Ther. 2023;18:1069-75.
- [CrossRef] [PubMed] [Google Scholar]






