Translate this page into:
Knowledge, attitudes and practices in the management of atopic dermatitis amongst allergists, dermatologists and pediatricians: A nation-wide survey
*Corresponding author: Leticia Freire Rautha, Department of Internal Medicine, Immunology Service, Federal University of Rio de Janeiro, Brazil. letrautha@hotmail.com
-
Received: ,
Accepted: ,
How to cite this article: Rautha LF, Lupi O, Valle SO. Knowledge, attitudes and practices in the management of atopic dermatitis amongst allergists, dermatologists and pediatricians: A nation-wide survey. Indian J Skin Allergy. 2025;4:57-65. doi: 10.25259/IJSA_2_2024
Abstract
Objectives
Atopic dermatitis (AD) is a chronic, inflammatory cutaneous disorder that presents with typical morphology and distribution of lesions. This disorder is commonly treated by dermatologists, allergists, and pediatricians. The objective of this study was to facilitate the integration of practices and attitudes in AD with physicians who most commonly treat this disease. Our study consisted of mapping medical knowledge in AD through research aimed at these three specializations.
Material and Methods
Using the electronic platform SurveyMonkey®, an online questionnaire about AD was created and sent to the participants’ digital media and E-mail by their respective national medical societies.
Results
Around, 1924 questionnaires were answered by dermatologists (41.8%), pediatricians (41.8%), and allergists (16.5%); the latter being those who achieved the highest average score (79.2% P < 0.0001). Question (Q) 13 was the one with the highest overall score (96.8%; P = 0.040), and the best pediatric performance (95.6%; P = 0.040). The one with the lowest overall score was Q19 (23.2%; P < 0.0001). Q30 achieved a higher score by allergists (92.4%; P < 0.0001), and dermatologists, Q21 (87.6%; P = 0.002).
Conclusion
The exchange of knowledge of AD among the three specialties can be beneficial in contributing to greater expertise in AD management, due to the possibility of a rich exchange of experiences between these professionals. Since this was an online survey, 100% participation could not be achieved.
Keywords
Atopic dermatitis
Attitudes
Knowledge
Practices
Questionnaires
Surveys
INTRODUCTION
Atopic dermatitis (AD) is a chronic inflammatory disease of the skin, with typical morphology and distribution of lesions, with intense itching as a characteristic feature.[1] AD, being a heterogeneous and chronic condition is characterized by erythematous to eczematous plaques with varying degrees of lichenification.[2] To facilitate both the integration of practices and attitudes in AD among the medical specialists who treat this disease the most, enabling the improvement of quality of care to the Brazilian population with AD, and to know the reality of medical knowledge in AD in the national territory, our study consisted of mapping medical knowledge in AD through national research aimed at allergists, dermatologists, and pediatricians.
Medical understanding regarding AD
A comparative study conducted in 2014 examined the primary international guidelines established by allergists/immunologists, dermatologists, and pediatricians, revealing discrepancies in the approaches employed by the various physician groups treating AD, as they adopt different strategies and consequently achieve varying outcomes.[3] The guidelines from several global organizations of allergists/immunologists, dermatologists, and pediatricians were compared, revealing that while there are similarities in established therapies and fundamental principles of AD, such as the use of emollients and topical corticosteroids, significant differences exist in recommendations, particularly concerning adjuvant therapies and auxiliary treatments, including preventive strategies for allergic triggers that exacerbate AD, which are more frequently implemented by allergists[3] [Table 1]. A French survey conducted in 2004 also assessed physicians’ knowledge and practices regarding the treatment of AD.[4] Barbarot and his team conducted telephonic interviews with a sample of 100 dermatologists, 100 pediatricians, 100 general practitioners, and 100 allergists. The survey aimed to create an inventory of reported practice intentions concerning AD among a representative sample of physicians, facilitating the assessment of future changes in practices following the release of new consensus recommendations for AD at the time of the survey. The study concluded that treatment modalities differ by specialty; specifically, only dermatologists utilize the full spectrum of topical corticosteroid activity levels for local treatment. Conversely, environmental and hygiene measures are frequently recommended similarly across all specialties. Notably, no general practitioner, dermatologist, or pediatrician systematically conducts food allergy testing, irrespective of the patient’s age. Allergists/immunologists are more likely to recommend substituting allergenic foods with alternatives.[4]
| Treatment | Guideline | Asia-pacific (APA) | ||
| Topical therapies | AAD | JTF | European | |
| TCS+TCI combination | Combination TCS and TCI therapy may be more effective than either alone | Not discussed | Contraindicates combined TCS and TCI therapy, concluding that it is not useful | Not discussed |
| “Dip and rub” technique | Soaking and smearing technique with TCS or TCI recommended | Soaking technique and smear with recommended moisturizers | Not discussed | Recommended soaking and smearing technique with TCS |
| Fear of corticosteroid use | Counseling on fear of corticosteroid use | Not discussed | Not discussed | Concerns about fear of corticosteroid use |
| Bleach baths | Effective as a therapy to decolonize Staphylococcus aureus | They are promising, but require more studies | May be helpful in reducing the severity of AD | Effective in AD patients who have secondary bacterial infection |
| Tar topical | There is insufficient data to recommend the topical use of tar | May be beneficial, but should not be used on skin with inflammation | Not discussed | Not discussed |
| Oral medications | Recommendations on dosage, adverse effects, follow-up, drug interactions, and contraindications of oral immunomodulatory therapies | Recommendations on dosage, adverse effects, initial and follow-up tests, drug interactions, and contraindications of oral therapies | Recommendations on dosage, adverse effects, initial and follow-up tests, drug interactions, and contraindications of oral therapies | Recommendations on dosage, adverse effects, initial and follow-up tests, drug interactions, and contraindications of oral therapies |
| Treatment | Guideline | Asia-pacific (APA) | ||
| Other recommendations | AAD | JTF | European | |
| Systemic therapy | ||||
| Antibiotics for secondary infection, with or without skin culture or without skin culture | Skin culture if initial antibiotic therapy fails | Suggested skin culture for methicillin-resistant S aureus before prescribing antibiotics initially | Not discussed | Not discussed |
| Silver-impregnated garments and silk garments | Effectiveness of silver or silk impregnated clothing is unclear | Silver or silk impregnated clothing can help patients | Clothes impregnated with silver or silk can help | Not discussed |
| Additives in the bath | There is not enough evidence to support bath additives | Bath additives such as oatmeal and baking soda) may have antipruritic effects | Not discussed | Emollient can be used during bathing |
| Vitamin D | There is no evidence to recommend the use of vitamin D | Recommends the use of vitamin D | There is not enough evidence to recommend the use of vitamin D | Not discussed |
| Environmental modifications | There is no evidence to support the laundry modifications; changes in temperature and humidity not discussed | Recommend environmental modifications (temperature and humidity control and laundry modifications) | It is recommended to avoid irritating fabrics and occlusive clothing | Not discussed |
| Treatment | Guideline | Asia-pacific (APA) | ||
| Topical therapies | AAD | JTF | European | |
| Allergen-specific immunotherapy | Testing required before indicated aeroallergen minimization; recommends only house mite covers | Recommends minimizing exposure to aeroallergens without testing and using covers and weekly washing of bedding and carpet removal | Supports minimization of exposure to house dust mites without testing | Not discussed |
| Aeroallergens | There is not enough evidence to support immunotherapy | Tests required before using immunotherapy for specific allergens | Tests required before using immunotherapy for specific allergens | Not discussed |
| Food allergy test | Recommends diagnostic elimination diet for 4–6 weeks or controlled oral food challenge if specific food allergy is clinically suspected | Recommends food-specific IgE testing if there is clinical suspicion of specific food allergy; oral food challenge only if IgE test results are negative | Recommends controlled oral food challenge if specific food allergy is clinically suspected | Not discussed |
| Treatment | Guideline | Asia-pacific (APA) | ||
| Other recommendations | AAD | JTF | European | |
| Systemic therapy | ||||
| Psychological care | Not discussed | Recommends psychological evaluation and treatment for patients with emotional distress if it is affecting treatment adherence | Psychosomatic counseling may be helpful for patients | Not discussed |
AAD: American academy of dermatology, JTF: Joint task force on practice parameters, APA: Asia pacific allergy, TCI: topical calcineurin-inhibitors, TCS: topical corticosteroids. Source: Adapted. IgE: Immunoglobulin E, AD: Atopic dermatitis
A subsequent study conducted in Cameroon assessed the knowledge, attitudes, and practices regarding the treatment of AD among physicians and other healthcare professionals. The findings revealed the following:[5]
A notable discrepancy when compared to the outcomes of the 2004 Enquête Nationale Française.
Interviewees struggled to define the chronic phase of AD.
There was an inability to establish the genetic associations related to the condition.
The study highlighted inadequate management practices for AD among the surveyed physicians and healthcare professionals.
There is a pressing need for the development of guidelines and the organization of regular continuing medical education sessions for healthcare professionals.[5]
The aforementioned findings underscore the necessity for further studies to enhance the understanding of best practices in managing AD, as well as the need to facilitate the integration of knowledge from diverse guidelines addressing the same condition.
MATERIAL AND METHODS
A nationwide cross-sectional study from August 2020 through August 2021 was conducted, using the SurveyMonkey® electronic platform. A questionnaire was prepared for online distribution, authored by the researchers, and built in two stages. The first stage consisted of 11 questions about the sociodemographic aspects of the participants, and the following variables were collected: Age, gender, medical specialty, profile of the place of care, educational level, and updated knowledge about AD (time since the participating physician last attended a lecture on AD, and the evaluation of self-knowledge in AD). The second stage included 20 questions addressing the major areas of knowledge in AD (epidemiology, pathophysiology, diagnostic methods, treatment, and complications), aligned with current consensus on the disease. The Likert scale served as a framework for formulating the questions, which were categorized based on their complexity: Questions of fundamental knowledge (the essential knowledge required for a physician to diagnose and treat a patient with AD at a basic level), questions of adequate knowledge (the knowledge necessary for a physician to diagnose and treat a patient with AD satisfactorily), and questions of desirable knowledge (the knowledge required for a physician to diagnose and treat a patient with AD with excellence) were delineated. For questions of fundamental knowledge, the primary topics presented in the introductions and abstracts of scientific articles related to AD, without a cutoff date, were considered during selection. For questions of adequate knowledge, recurring themes from bibliographic review articles on AD, also without a cutoff date, were utilized. In contrast, for questions of desirable knowledge, topics exclusively addressed in systematic reviews of the literature from the past 4 years were selected, in addition to information from the principal national and international consensuses on AD. The subject descriptor “AD” was employed, utilizing electronic data from journals indexed in the National Library of Medicine (MEDLINE - PubMed) and the Scientific Library Online. The questionnaire was applied to allergists, dermatologists, and pediatricians, being distributed by the respective medical societies, the Associação Brasileira de Alergia e Imunologia (ASBAI), the Sociedade Brasileira de Dermatologia (SBD), and the Sociedade Brasileira de Pediatria (SBP). The questionnaire was also sent by the authors to the social media profiles of the medical specialists. The sample calculation was based on a study conducted in 2018, by the Federal University of São Paulo (UNIFESP), on Brazilian medical demography.[6] It was considered that a representative sample should include at least 800 pediatricians, 800 dermatologists, and 300 allergists. For data analysis, the Chi-square test (χ2) (association between sociodemographic variables, and correct answer of the survey with the specialty) and the adjusted χ2 were performed, at the level of 1.7%, aiming to control the type I error (α error), and analysis of variance (one-way) followed by Tukey’s multiple-way comparison test.
RESULTS
Approximately 20,000 surveys were distributed to medical specialists through Email and social media. Of these, 2635 participants consented to engage in the study, with 73%, or 1924 respondents, completing the survey in its entirety. For the total sample, 1924 questionnaires were included (73% of the 2,635 surveys), all of which were fully answered, comprising: 804 (41.8%) from dermatology; 803 (41.7%) from pediatrics; and 317 (16.5%) from immunology [Figure 1]. Allergy was the specialty with the highest mean score in our test, presenting a percentage of 79.2% of correct answers [Table 2]. Dermatologists had the second highest score, with an average of 68.9%, and pediatricians had 61.0%. Our findings found that specialists who had been recently updated in their understanding of AD achieved a higher percentage of correct answers as compared to those who had not attended any recent academic sessions on AD [Table 3]. Regarding the self-assessment of the participating physicians, there was a confirmation of the individual perception of personal knowledge in AD. Consequently, individuals who regarded their knowledge as excellent achieved the highest average percentage of correct responses, while the participants’ scores diminished as they were assigned a lower self-assessment [Table 3]. Dermatology and immunology had a higher percentage of physicians with a specialist degree (48.8% and 48.3%, respectively), with immunology having the highest percentage of physicians with master’s degrees (15.8%) and Doctor of Philosophy (9.1%) [Table 3]. Allergists considered themselves the most updated (<6 months) with 83.6% compared to 53.7% of dermatologists and 35% of pediatricians [Table 3]. Of the allergists participating in the study, 11% answered that they had university affiliations and were most related to the academic environment. According to our study of the questionnaire’s second stage, Q13 (“The prevalence of AD is higher in:”) had the greatest overall percentage of accurate answers (96.8%), followed by Q18 (“The typical clinical picture of AD is characterized by:”), which had 95.7% accurate answers. Both questions were regarded as essential AD information [Table 4]. Q19 (“What can we not associate the pathogenesis of pruritus in AD to?”) and Q25 (“In the healthy skin of patients with AD we can observe, except:”) had the lowest mean percentage of accurate responses (23.2% and 32.2%, respectively) [Table 4]. Allergists had a higher percentage of correct answers in Q30 (“Dupilumab is an immunobiological drug, recently approved by the FDA for the treatment of AD. Regarding its mechanism of action, it prevents which substances from binding to its target receptors?”) and Q24 (“What are the main allergens participating in the etiopathogenesis of atopic dermatitis?”), scoring 92.4% and 89%, respectively. Dermatologists had a higher percentage of correct answers in Q21 responses (“Which of the following statements is false in relation to the use of moisturizers in the treatment of atopic dermatitis?”) and Q22 responses (“Regarding the use of topical corticosteroids in the treatment of atopic dermatitis, we can state that:”), with 87.6% and 77.6%, respectively. Pediatricians coincided with the best performance in the questionnaire precisely in the questions with the best overall score of our study, questions 13 and 18, respectively [Table 4].
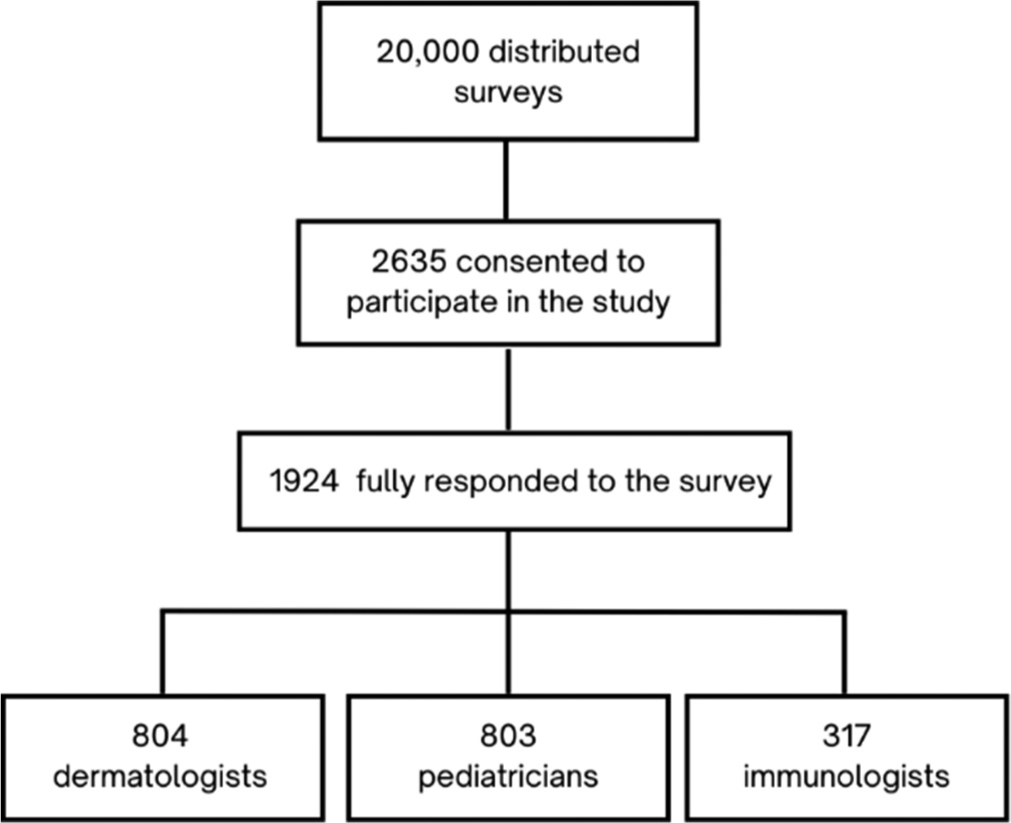
- Organisation chart of questionnaire responses.
| Sample | n | Average | SD | Median |
|---|---|---|---|---|
| Total | 1924 | 67.3 | 14.9 | 68.4 |
| Allergists | 317 | 79.2 | 11.7 | 78.9 |
| Dermatology | 804 | 68.9 | 14.1 | 68.4 |
| Pediatrics | 803 | 61.0 | 13.4 | 63.2 |
SD: Standard deviation, Bold values: Medical specialty with highest mean score in the test.
| Variable | Total | Dermatology (E1) | Pediatrics (E2) | Allergists (E3) | P-valuea | Significant differencesb | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | |||
| Schooling | ||||||||||
| Doctor of philosophy | 70 | 3.6 | 19 | 2.4 | 22 | 2.7 | 29 | 9.1 | ||
| Masters | 207 | 10.8 | 87 | 10.8 | 70 | 8.7 | 50 | 15.8 | <0.0001 | E1≠E2≠E3 |
| Expert | 847 | 44.0 | 392 | 48.8 | 302 | 37.6 | 153 | 48.3 | ||
| Residency+graduation | 800 | 41.6 | 306 | 38.1 | 409 | 50.9 | 85 | 26.8 | ||
| Works most of the time | ||||||||||
| Private/polyclinic clinic | 1184 | 61.5 | 662 | 82.3 | 326 | 40.6 | 196 | 61.8 | <0.0001 | E1≠E2≠E3 |
| Private hospital | 156 | 8.1 | 24 | 3.0 | 110 | 13.7 | 22 | 6.9 | ||
| Public hospital | 345 | 17.9 | 53 | 6.6 | 240 | 29.9 | 52 | 16.4 | ||
| Basic Health Unit | 132 | 6.9 | 40 | 5.0 | 82 | 10.2 | 10 | 3.2 | ||
| Private/public university | 107 | 5.6 | 25 | 3.1 | 45 | 5.6 | 37 | 11.7 | ||
| Preferred work activity | ||||||||||
| Care | 1731 | 90.0 | 731 | 90.9 | 731 | 91.0 | 269 | 84.9 | 0.0001 | E1≠E3 e E2≠E3 |
| Undergraduate teacher | 73 | 3.8 | 15 | 1.9 | 35 | 4.4 | 23 | 7.3 | ||
| Lecturer in postgraduate/Advisor professor | 68 | 3.5 | 36 | 4.5 | 16 | 2.0 | 16 | 5.0 | ||
| Health management | 52 | 2.7 | 22 | 2.7 | 21 | 2.6 | 9 | 2.8 | ||
| Update in AD | ||||||||||
| <6 months | 978 | 50.8 | 432 | 53.7 | 281 | 35.0 | 265 | 83.6 | <0.0001 | E1≠E2≠E3 |
| up to 2 years | 588 | 30.6 | 252 | 31.3 | 291 | 36.2 | 45 | 14.2 | ||
| >2 years/don’t remember | 358 | 18.6 | 120 | 14.9 | 231 | 28.8 | 7 | 2.2 | ||
| Personal knowledge about AD | ||||||||||
| Insufficient | 47 | 2.4 | 13 | 1.6 | 30 | 3.7 | 4 | 1.3 | <0.0001 | E1≠E2≠E3 |
| Regular | 374 | 19.4 | 117 | 14.6 | 242 | 30.1 | 15 | 4.7 | ||
| Good | 1271 | 66.1 | 575 | 71.5 | 490 | 61.0 | 206 | 65.0 | ||
| Great | 232 | 12.1 | 99 | 12.3 | 41 | 5.1 | 92 | 29.0 | ||
The data were expressed by frequency (n) and percentage (%). (a) General χ2test. (b) significant differences according to the adjusted statistical test, at the level of 1.7% (comparison 2 to 2), AD: Atopic dermatitis, Bold values: Higher level of education and academic interest on the part of allergists. Identification of notable distinctions among the three medical specialties.
| Survey question | Correct answer | Total | Dermatology | Pediatrics | Immunology | ||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | n | % | ||
| Q13: The prevalence of atopic dermatitis is higher in: | ✓ Children | 1863 | 96.8 | 786 | 97.8 | 768 | 95.6 | 309 | 97.5 |
| Q14: Atopic dermatitis is characterized by | ✓ Immune activation and epithelial barrier dysfunction | 1821 | 94.6 | 767 | 95.4 | 738 | 91.9 | 316 | 99.7 |
| Q15: Which of the following signs or symptoms is NOT suggestive of atopic dermatitis? | ✓ Pain | 1811 | 94.1 | 767 | 95.4 | 740 | 92.2 | 304 | 95.9 |
| Q16: Is it considered major criterion for the diagnosis of atopic dermatitis? | ✓ Personal or/and family history of atopy | 1004 | 52.2 | 426 | 53.0 | 422 | 52.6 | 156 | 49.2 |
| Q17: Which of the following factors is NOT considered a trigger for worsening atopic dermatitis? | ✓ Use of soaps with low pH | 945 | 49.1 | 417 | 51.9 | 345 | 43.0 | 183 | 57.7 |
| Q18: The typical clinical picture of atopic dermatitis is characterized by | ✓ Erythema. Flaking in areas of flexure and itching | 1842 | 95.7 | 783 | 97.4 | 749 | 93.3 | 310 | 97.8 |
| Q19: What cannot we associate the pathogenesis of pruritus in atopic dermatitis? | ✓ Inhibition of IL31 | 446 | 23.2 | 173 | 21.5 | 137 | 17.1 | 136 | 42.9 |
| Q20: It is considered the most relevant and frequent pathogen responsible for aggravating an atopic dermatitis | ✓ Staphylococcus aureus | 1659 | 86.2 | 742 | 92.3 | 618 | 77.0 | 299 | 94.3 |
| Q21: Which of the following statements is false in relation to the use of moisturizers in the treatment of atopic dermatitis? | ✓ Do not change the intensity of itching | 1629 | 84.7 | 704 | 87.6 | 654 | 81.4 | 271 | 85.5 |
| Q22: Regarding the use of topical corticosteroids in the treatment of atopic dermatitis. we can state that | ✓ Controls itching and eczematous lesions | 1368 | 71.1 | 625 | 77.7 | 503 | 62.6 | 240 | 75.7 |
| Q23: Are filaggrin gene changes associated with the following findings in atopic dermatitis, except? | ✓ Increased ceramide production | 1059 | 55.0 | 539 | 67.0 | 300 | 37.4 | 220 | 69.4 |
| Q24: What are the main allergens participating in the etiopathogenesis of atopic dermatitis? | ✓ Mites, milk and egg | 1484 | 77.1 | 558 | 69.4 | 615 | 76.6 | 311 | 98.1 |
| Q25: On the apparently healthy skin of patients with atopic dermatitis we can observe, except | ✓ Greater diversity of the microbiota | 619 | 32.2 | 230 | 28.6 | 243 | 30.3 | 146 | 46.1 |
| Q26a e Q26b: If you answered yes, which statement best defines this score? | ✓ It’s a gravity score | 1194 | 62.1 | 494 | 61.4 | 418 | 52.1 | 282 | 89.0 |
| Q27: In patients diagnosed with atopic dermatitis, refractory to treatment, which should NOT be considered | ✓ Low serum vitamin B12 levels | 1467 | 76.2 | 630 | 78.4 | 541 | 67.4 | 296 | 93.4 |
| Q28: Regarding the use of systemic immunomodulators in atopic dermatitis (AD), we can state that | ✓ Cyclosporine is potentially nephrotoxic | 1053 | 54.7 | 545 | 67.8 | 257 | 32.0 | 251 | 79.2 |
| Q29: About complementary tests on atopic dermatitis, what can we say? | ✓ The specific IgE dosage assesses allergen awareness | 1411 | 73.3 | 566 | 70.4 | 550 | 68.5 | 295 | 93.1 |
| Q30: Dupilumab is an immunobiological drug, recently approved by the FDA for the treatment of atopic dermatitis. Regarding its mechanism of action, it prevents which substances from binding to its target receptors? | ✓ IL-4 e IL-13 | 1061 | 55.1 | 417 | 51.9 | 351 | 43.7 | 293 | 92.4 |
| Q31: On the complications in atopic dermatitis (AD), we can state that | ✓ Exfoliative erythromycin may be related to Staphylococcus spp. infections. | 867 | 45.1 | 352 | 43.8 | 361 | 45.0 | 154 | 48.6 |
The data were expressed by frequency (n) and percentage (%). IgE: Immunoglobulin E, FDA: Food and drug administration, IL: Interleukin, Q26a: Does doctor know the term SCORAD (Scoring Atopic Dermatitis)?
Note: Questions 1 through 12 pertained to the initial stage of the study questionnaire, with the consent form as the first question, followed by questions 2 to 12, which gathered personal and professional information from the research participants.
DISCUSSION
AD is commonly treated by dermatologists, allergists, and pediatricians. Although physicians are not fully aware of the guidelines created by specialized organizations other than their own, the knowledge and updating of these professionals on AD are fundamental to ensuring a good quality of life for patients with this disease.[3,7] In our study, we can attribute three factors to allergists having performed the highest score in our questionnaire among the three medical specialties researched: the higher education of allergists (higher percentage of master’s and Doctor of Philosophy degrees), attachment, and affiliation in teaching institutions, and recent participation in any academic event associated with AD. In the three variables mentioned above in the questionnaire, it can be assumed that concerned participants are inclined to update themselves academically. Regarding the self-assessment of the participating physicians, there was a confirmation of the individual perception of their knowledge in AD due to a proportional relationship of this with the performance in our survey, thus demonstrating the interest of parties in this research by responding correctly and sincerely [Table 5]. In the analysis of the second stage of the questionnaire, we observed that the questions with the highest general percentage of correct answers (Q13 and Q18) (areas of knowledge in epidemiology and pathophysiology, respectively) can be considered fundamental knowledge of AD because both its prevalence in the infantile age group and the clinical characteristic of eczema related to allergic mechanisms (questions themes) can be identified in the scientific literature since 1933 as the description of AD.[8-10] The questions with the most correct answers by allergists were Q30 and Q24 (areas of knowledge in diagnostic methods and treatment, respectively), which involve the management and immunopathological knowledge of AD, with atopic hypersensitivity being an important cause of eczematous eruptions in this disease.[8] Although dupilumab operates through an immune-mediated mechanism,[11] which may enhance its familiarity among allergists and immunologists, it has garnered significant global attention. This drug has been extensively described and promoted by numerous specialty organizations, including Brazilian entities such as SBD, ASBAI, and SBP.[1,12] We also observed that the questions with the highest percentage of correct answers from dermatologists were Q21 and Q22 (areas of knowledge in treatment). Both address the practice in the therapy of AD with topical medications. Studies show that dermatologists base their management of AD on skin hydration, the use of topical anti-inflammatory drugs, the prevention of triggering factors, and educational programs.[1,13,14] The lowest percentage of correct answers from dermatologists was in Q24 and may be related to a less common practice of these specialists to allergic tests. According to a study conducted with eighteen specialists with experience in AD, indicated by SBD, 89% reported not performing the prick test or RAST as part of their routine evaluation in patients of AD.[1] The questions with the highest percentage of correct answers in pediatrics were also those with the highest overall score of this study (Q13 and Q18), which had as their central theme, basic concepts of AD (the essential knowledge required for a physician to effectively diagnose and manage a patient with AD at a fundamental level).[4] A hypothesis for pediatricians to have scored less in our test among the three specialties can be that pediatricians have a common practice of referring the most severe cases of AD to dermatology. In general, pediatricians do not have the practice in second-line treatments and the necessary knowledge to deal with a more resistant and prolonged AD. Our study pioneered the evaluation of medical knowledge on AD in Brazil through an online survey. Our research, highlights the importance of continuously updating the academic knowledge of medical specialists to ensure optimal management and therapeutic approach for AD. Brazilian allergists not only demonstrated strong performance across all areas assessed in our study but also exhibited greater expertise in managing and prescribing therapies related to immunoallergic mechanisms. Dermatologists, in contrast, had a deeper understanding of AD management, particularly regarding medications and topical therapies. Pediatricians displayed solid knowledge of the fundamental characteristics that define AD. However, dermatologists and pediatricians lacked the level of expertise that allergists had in allergy testing and the use of immunobiological drugs.
| Variable | n | Percentage of correct answers in the questionnaire |
|---|---|---|
| Average±SD | ||
| Update on AD | ||
| 1 | ||
| <6 months | 978 | 72.3±14.2 |
| 2 | ||
| up to 2 years | 588 | 64.1±13.4 |
| 3 | ||
| > 2 years/do not remember | 358 | 58.9±13.4 |
| Personal knowledge about AD | ||
| 1 | ||
| Insufficient | 47 | 55.6±14.3 |
| 2 | ||
| Regular | 374 | 59.6±13.7 |
| 3 | ||
| Good | 1271 | 68.3±14.2 |
| 4 | ||
| Great | 232 | 76.5±13.0 |
SD: Standard deviation, AD: Atopic dermatitis
CONCLUSION
We conclude that the exchange of medical knowledge on AD among the three specialties examined in this study, present both in the training courses of medical specialists and, in academic meetings, can be beneficial in contributing to a greater expertise of allergists, dermatologists, and pediatricians in their management of AD, due to the possibility of a rich exchange of experiences between these professionals. Empowering these medical professionals to manage their patients with more complete AD knowledge might improve the quality of life of patients and also upgrade medical education in AD.
Ethical approval
The research/study was approved by the Institutional Review Board at Research Ethics Committee of the Federal University of Rio de Janeiro, number 33551420.2.0000.5257, dated 08th July, 2021.
Declaration of patient consent
Although the research was not conducted with a sample of patients but rather with volunteer medical professionals, the authors affirm that they obtained all necessary consent from the physicians involved in the study.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Consensus on the therapeutic management of atopic dermatitis-Brazilian Society of Dermatology. An Bras Dermatol. 2019;94:67-75.
- [CrossRef] [PubMed] [Google Scholar]
- Practical guide to updating in atopic dermatitis-Part I: Etiopathogenesis, clinical and diagnosis. Joint position of the Brazilian Association of Allergy and Immunology and the Brazilian Society of Pediatrics. Arq Asthma Alerg Imunol. 2017;1:131-56.
- [Google Scholar]
- Comparison of dermatology and allergy guidelines for atopic dermatitis management. JAMA Dermatol. 2015;151:1009-13.
- [CrossRef] [PubMed] [Google Scholar]
- The management of atopic dermatitis in children by dermatologists, paediatricians, general practitioners and allergologists: A national survey on practice patterns. Ann Dermatol Venereol. 2005;132(Spec No 1):1S283-95.
- [CrossRef] [Google Scholar]
- Knowledge, attitudes and practices of the medical personnel regarding atopic dermatitis in Yaoundé, Cameroon. BMC Dermatol. 2017;17:1.
- [CrossRef] [PubMed] [Google Scholar]
- Medical demography in Brazil-2018 In: São Paulo: Department of Preventive Medicine, Faculty of Medicine, University of São Paulo, Federal Council of Medicine, Regional Council of Medicine. 2018. p. :287.
- [Google Scholar]
- Patterns of clinical management of atopic dermatitis in infants and toddlers: A survey of three physician specialties in the United States. J Pediatr. 2013;163:1747-53.
- [CrossRef] [PubMed] [Google Scholar]
- Current guidelines for the evaluation and management of atopic dermatitis: A comparison of the Joint Task Force Practice Parameter and American Academy of Dermatology guidelines. J Allergy Clin Immunol. 2017;139:S49-57.
- [CrossRef] [PubMed] [Google Scholar]
- The history of atopic dermatitis. Clin Dermatol. 2017;35:344-8.
- [CrossRef] [PubMed] [Google Scholar]
- Atopic dermatitis/atopic eczema. Chem Immunol Allergy. 2014;100:81-96.
- [CrossRef] [PubMed] [Google Scholar]
- Update on atopic dermatitis: Diagnosis, severity assessment, and treatment selection. J Allergy Clin Immunol Pract. 2020;8:91-101.
- [CrossRef] [PubMed] [Google Scholar]
- Practical guide to updating atopic dermatitis - Part II: Therapeutic approach In: Joint Position Statement of the Brazilian Association of Allergy and Immunology and the Brazilian Society of Pediatrics. 2017.
- [Google Scholar]
- A study on the knowledge, attitudes and practices of Southeast Asian dermatologists in the management of atopic dermatitis. Ann Acad Med Singap. 2006;35:794-803.
- [CrossRef] [PubMed] [Google Scholar]
- Different approaches to atopic dermatitis by allergists, dermatologists, and pediatricians. Dermatol Res Pract. 2021;2021:6050091.
- [CrossRef] [PubMed] [Google Scholar]







