Translate this page into:
Angina bullosa hemorrhagica: A case series of a rare entity
*Corresponding author: Divyanshu Deshmukh, Department of Dermatology, Venereology and Leprosy, Government Multispecialty Hospital, Chandigarh, India. divya.deepdeshmukh@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Kaur S, Kaur S, Deshmukh D. Angina bullosa hemorrhagica: A case series of a rare entity. Indian J Skin Allergy. 2025;4:78-80. doi: 10.25259/IJSA_33_2024
Abstract
The term “Angina bullosa hemorrhagica” (ABH) refers to the sudden emergence of oral blood-filled vesicles and bullae that are not related to systemic illnesses, vesiculobullous disorders, blood dyscrasia, or any other recognized cause. It presents as sudden-onset hemorrhagic bullae that burst spontaneously, causing superficial erosions that heal on their own without leaving any scarring in a few days. The most frequently recognized triggering factor seems to be trauma; however, the fundamental tissue abnormality is still unknown. In this report, we are presenting three cases diagnosed clinically as ABH in an effort to highlight this rare cause of oral hemorrhagic bullae, which is a self-limiting disease.
Keywords
Angina bullosa hemorrhagica
Hemorrhagic bulla
Self-limiting bulla
Trauma
INTRODUCTION
Blood dyscrasia, systemic illnesses, and vesiculobullous disorders are the main causes of oral bullae. Angina bullosa hemorrhagica (ABH), a name originally proposed by Badham in 1967, is one uncommon cause of oral bullae.[1] This uncommon condition is marked by blood-filled subepithelial bullae in the oral or oropharyngeal mucosa in the absence of any systemic, hematological, or dermatological conditions.[2]
In the field of dermatology, understanding ABH is essential to prevent misdiagnosis because the condition heals on its own without any medical intervention. We report three cases of ABH due to its rarity and spontaneous resolution.
CASE REPORT
Case 1
A 50-year-old female presented to our Dermatology and Venereology outpatient clinic with a chief complaint of multiple blood-filled lesions on the dorsum of the tongue and bilateral buccal mucosa and palate for the last 2 days. The lesions were asymptomatic, and there was no history of any similar episodes in the past or of recent drug intake. There were no other systemic complaints. On dermatological examination, there were multiple, discrete, tense, dark red-colored hemorrhagic bullae ranging in size from 0.5 cm to 2 cm over the dorsum of the tongue, hard palate, and bilateral buccal mucosa [Figure 1a]. The patient was advised hematological investigations, including coagulation profile, and the findings were within normal limits, and viral markers were also non-reactive. A provisional diagnosis of ABH was made. To rule out oral pemphigus, oral lichen planus, and fixed drug eruption, the patient was advised biopsy, but she was not willing for the same. The lesions healed within a few days without any scarring [Figure 1b].
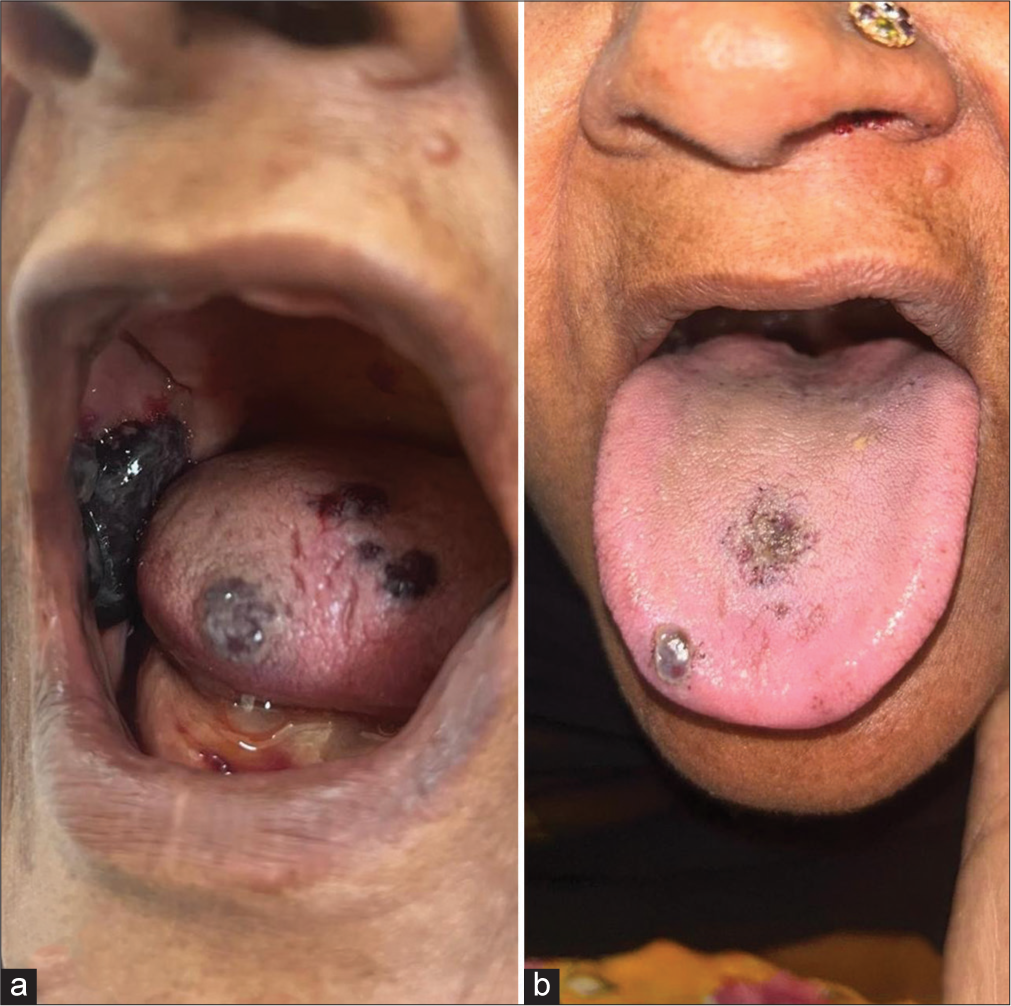
- (a) Multiple hemorrhagic bullae over buccal mucosa and dorsum of tongue. (b) The lesions resolved spontaneously within a few days (Case 1).
Case 2
A 56-year-old female presented to our Dermatology and Venereology outpatient clinic with a chief complaint of sudden onset of a single, blood-filled lesion over the lateral margin of her tongue for 1 day. It was associated with a mild burning sensation. She mentioned that she had been having these kinds of lesions a few. times a year since her symptoms commenced 3 years prior. She correlated the onset with the intake of spicy food and hot beverages. It was not associated with any systemic illness. After each episode, the lesion healed spontaneously, so she did not seek any treatment. On dermatological examination, a single, well-defined hemorrhagic bulla of size 2 cm was present over the left lateral aspect of the tongue [Figure 2]. All her blood investigations were within normal limits, and viral markers were non-reactive. The lesions healed spontaneously within 3 days without any residual scarring.

- Single hemorrhagic bulla over the left lateral aspect of the tongue (Case 2).
Case 3
A 33-year-old female presented to our outpatient clinic with a single blood-filled lesion over the lateral aspect of the tongue for the past 2 days. It was associated with mild pain. There was no associated comorbidity or drug history. There was no history of any hormonal irregularities or flare-up of lesions with the menstrual cycle. However, across the lesion area, there was a history of inadvertent tongue bite. She also recalled a similar episode occurring a few years ago, that resolved on its own without any treatment. On examination, a single hemorrhagic bulla was present over the left lateral aspect of the tongue [Figure 3a]. All her blood investigations were normal. The lesion healed spontaneously within 3–4 days [Figure 3b].

- (a) Single, tense hemorrhagic bulla over the left lateral aspect of the tongue. (b) The lesion healed on its own within a few days (Case 3).
DISCUSSION
There is no well-accepted root cause for ABH. However, it is considered to occur after any physical trauma, which could include hot and spicy food consumption, coughing or sneezing, and dental procedures.[3] It is also associated with diabetes mellitus, hypertension, and steroid inhalation.[4] There was no history of long-term steroid inhaler use in any of our cases. A subepithelial hemorrhagic bullae forms because of trauma-induced disruption of the epithelial-connective-tissue interface, which leads to superficial capillary bleeding.[5]
In two of our cases, where the patients mentioned links between ABH, hot and spicy food, and local trauma, we were able to pinpoint the trigger. It presents as a red-purple-colored bulla over the hard/soft palate, tongue, or buccal mucosa. The blisters only last a few days before spontaneously rupturing to leave a superficial ulcer that heals without pain, discomfort, or scarring. As was observed in all our three cases, the blisters are short-lived, last only a few days and heal painlessly without leaving any scars. However, recurrent lesions are reported.[6]
Diagnosis of ABH is mainly clinical; Ordioni., in 2019, proposed the following diagnostic criteria for ABH:[7]
Hemorrhagic bulla or erosion with a history of bleeding in the oral mucosa
Exclusively oral or oropharyngeal localization
Palatal localization
A triggering event
Recurrent lesions
Favorable evolution without a scar within a few days
Painless lesion or a tingling or burning sensation.
Normal platelets count and coagulation test results
Negative DIF results.
Six criteria (including the first and second) should be met to diagnose ABH. Since each of our cases met more than six criteria, they were all considered to satisfy the diagnostic criteria. Histopathology may reveal subepithelial separation from the lamina propria with inflammatory infiltrate. To exclude other hematological disorders that mimic ABH, thorough blood analysis, including complete blood count and coagulation profile, is essential. In all our cases, the results of these tests were unremarkable.
We considered the following differential diagnoses: thrombocytopenia, oral lichen planus, fixed drug eruption, and pemphigus vulgaris. However, there were no skin lesions, no history of any drug intake, and no coagulation profile abnormalities, so these possibilities were ruled out.
No treatment is required for ABH, as it heals spontaneously. Patients were counseled to refrain from potential triggers and maintain good oral hygiene. Symptomatic treatment, including topical antiseptics and mouthwash, was advised.
CONCLUSION
ABH is a benign, self-limiting, and under-reported disease that should be kept in differential diagnoses of blood-filled lesions in the oral cavity, as it can prevent misdiagnosis and unnecessary treatment.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Blood blisters and the oesophageal cast. J Laryngol Otol. 1967;81:791-803.
- [CrossRef] [PubMed] [Google Scholar]
- Angina bullosa haemorrhagica an enigmatic oral disease. World J Stomatol. 2015;4:1-7.
- [CrossRef] [Google Scholar]
- Oral blood blisters in angina bullosa haemorrhagica secondary to trauma of eating and dental injection. Br Dent J. 1988;165:286-7.
- [CrossRef] [PubMed] [Google Scholar]
- Angina bullosa haemorrhagica: A complication of long-term steroid inhaler use. Br Dent J. 1988;165:176-9.
- [CrossRef] [PubMed] [Google Scholar]
- Oral blood blisters: Angina bullosa haemorrhagica. Br J Oral Maxillofac Surg. 1985;23:9-16.
- [CrossRef] [PubMed] [Google Scholar]
- Angina bullosa haemorrhagica presenting as acute upper airway obstruction. Br J Anaesth. 2004;92:283-6.
- [CrossRef] [PubMed] [Google Scholar]
- Angina bullosa haemorrhagica: A systematic review and proposal for diagnostic criteria. Int J Oral Maxillofac Surg. 2019;48:28-39.
- [CrossRef] [PubMed] [Google Scholar]






