Translate this page into:
Allergic contact dermatitis in children with atopic cheilitis and eyelid dermatitis – A case series
*Corresponding author: Shatabdee Sahoo, Department of Dermatology, IMS and SUM Hospital, Bhubaneswar, Odisha, India. shatabdeesssahoo@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Pramanik A, Sahoo S, Panda M, Jena AK. Allergic contact dermatitis in children with atopic cheilitis and eyelid dermatitis – A case series. Indian J Skin Allergy. 2025;4:81-4. doi: 10.25259/IJSA_49_2024
Dear Editor,
Allergic contact dermatitis (ACD) is a delayed hypersensitivity reaction to an allergen in previously sensitized individuals. It presents with reddish oozy-to-scaly lesions associated with itching or burning sensation within a few days of exposure. The prevalence of ACD is about 16.5% in children and adolescents, thereby making it a growing concern in the pediatric population.[1] Atopic dermatitis (AD) is a chronic pruritic condition characterized by a relapsing-remitting course and can present with varying morphology and distribution depending on age. Children present predominantly with flexural lesions; however, involvement of periorbital and perioral area is common. The face has delicate skin, making it more accessible for contact with various airborne allergens and allergens carried by the hands. Skin barrier disruption in AD, being the main pathology, predisposes them to develop ACD. Hence, recurrent chronic eyelid and lip dermatitis in AD patients necessitates patch testing to rule out ACD. We hereby present a series of 6 patients with AD who presented with eyelid dermatitis and cheilitis and had patch test positivity.
A series of six patients (4 females and 2 males) presented to the outpatient department with itchy, erythematous, scaly plaques over the face, mostly involving the periorbital and perioral areas, which were associated with oozing and lichenification [Figures 1-2]. The lesions had a chronic relapsing course with recurrent episodes. The duration of the disease varied from 5 months to 2.5 years. On clinical assessment, the children were diagnosed with AD based on the fulfillment of Hanifin and Rajka criteria. A detailed history was taken, and a thorough examination was performed to rule out seborrheic dermatitis, photosensitive eczema, tinea faciei, ocular rosacea, and lip-lickers cheilitis. There was no history of prolonged application of topical corticosteroids. The chronic nature of the lesions raised substantial doubt about an allergic etiology. However, the history of any specific allergens could not be recalled by the parents. All patients underwent routine laboratory investigations, including total serum immunoglobulin E (IgE) and absolute eosinophil count (AEC). 5 out of the 6 children showed raised serum IgE, 2 patients had increased eosinophil count (AEC), and the rest of the investigations were unremarkable [Table 1].

- Hyperpigmented scaly plaques over eyelids and photosensitive eczema over cheek of a 9-year-old male patient.

- Erythematous scaly plaques over lips and perioral areas of a 12-year-old female patient.
| No. | Age/gender | Disease duration | Presentation | Relevant history of atopy | Serum IgE levels (IU/mL) | Serum AEC levels (per cu.mm) | Allergen detected | Intensity of reaction |
|---|---|---|---|---|---|---|---|---|
| 1 | 8 years/F | 9 months | Eyelid dermatitis | Pityriasis alba, Dennie Morgan folds, history of allergic rhinitis | 677 (Raised) | 250 (Normal) | Nickel sulfate (ISB -7) | 1+ (weak positive) |
| 2 | 9 years/M | 1.5 years | Eyelid dermatitis | Hyper linearity of palms, prurigo like lesions over bilateral legs, atopic dirty neck, history of asthma | 345.6 (Raised) | 204 (Normal) | Fragrance mix (ISB-17), hexamine (COS-27) | 1+ (weak positive) |
| 3 | 12 years/F | 2 years | Lip cheilitis | Generalized xerosis, hyperlinear palm, history of allergic rhinitis, family history of atopy | 122.25 (Normal) | 432 (Normal) | Nickel (ISB-7) | 2 + (strong positive) |
| 4 | 7 years/F | 5 months | Eyelid+lip dermatitis | Palmer hyper linearity, pityriasis alba and wide spread xerosis | 2567.3 (Raised) | 1800 (Raised) | Nickel (ISB-7), colophony (ISB-9) | 1+ (weak positive) |
| 5 | 10 years/F | 1.5 years | Lip cheilitis+eyelid dermatitis | Dennie Morgan folds, atopic dirty neck, history of asthma | 1267.2 (Raised) | 300 (normal) | Nickel (ISB-7), thiomersal (COS-22) | 1+ (weak positive) |
| 6 | 15 years/M | 2.5 years | Eyelid dermatitis | Flexural eczema, hyperlinearity of palms, keratosis pilaris, family history of asthma | 1054 (Raised) | 640 (raised) | Potassium dichromate (ISB-6) | 1+ (weak positive) |
IgE: Immunoglobulin E, AEC: Absolute eosinophil count, COS: Cosmetic series, ISB: Indian standard battery
Patch test was performed with Indian standard series (ISS) of 20 allergens and Cosmetic series of 32 allergens. Supplementary patches of suspected products and substances such as face creams, body creams, kajal, cosmetics, body spray, perfumes, lip balms, lipsticks, toothpaste, sunscreens, and scrapings from spectacles were combined with liquid paraffin and were applied [Figure 3]. Patch test interpretation was done according to International Contact Dermatitis Research Group criteria. Readings were taken after 48 and 96 h (on Days 2 and 4), and patients with high suspicion of contact allergy to topical medication were followed up after 7 days [Figure 4]. All the children showed positive reactions to one or more allergens after the first follow-up, with nickel being the most common culprit. No patient developed any delayed positivity on day 7. Moreover, there was no positive reaction to any of the supplementary agents. The parents were explained about the possible reaction and advised about a list of allergen-containing products to avoid. The children were prescribed topical corticosteroids for 7 days, followed by calcineurin inhibitors for a month, with complete resolution of the lesions. In the subsequent follow-ups for 3 months, there were no relapses after cautious avoidance of the suspected allergens by the patient and his family members, thereby signifying a probable association of allergic contact with lip and eyelid dermatitis.
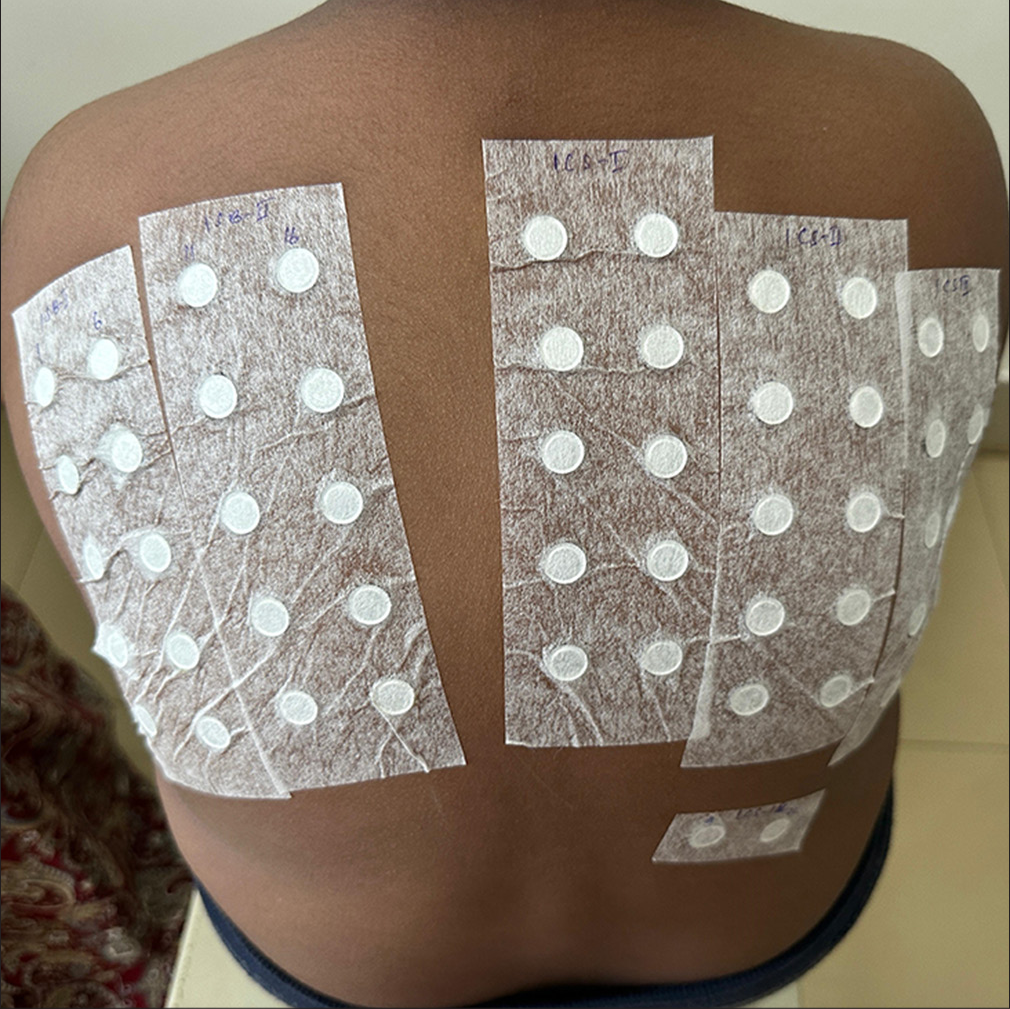
- Patch test performed with Indian standard series and cosmetic series over upper back.
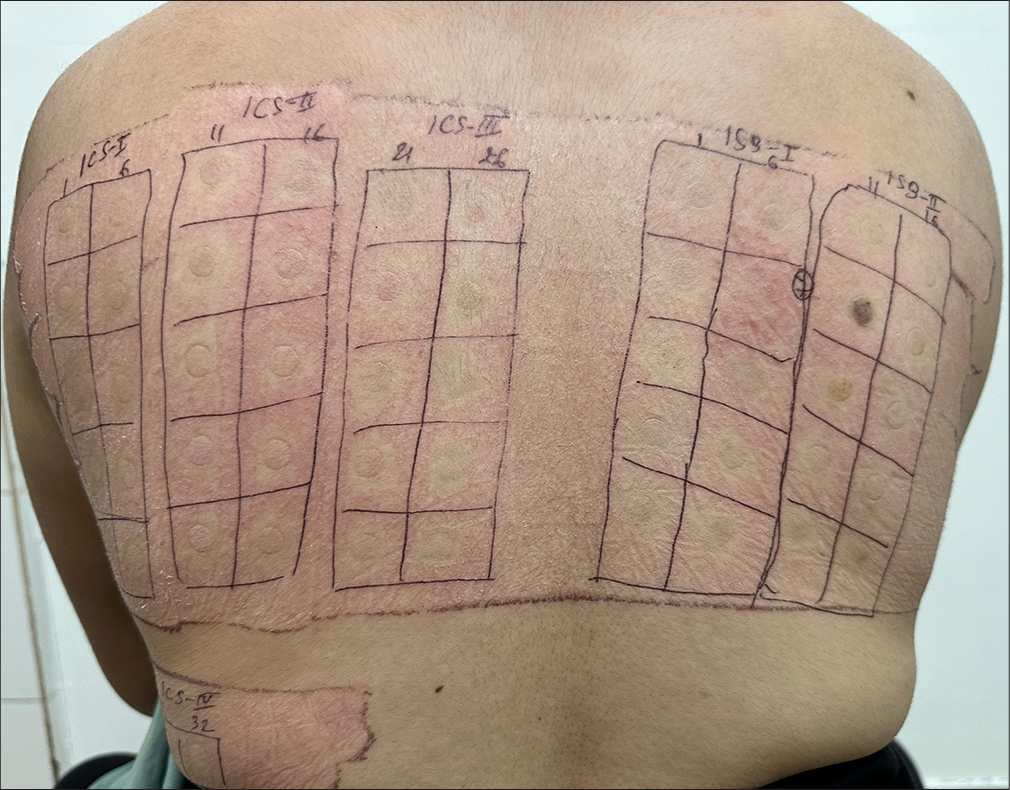
- Patch test showing positive test for nickel sulfate (Indian standard series-7).
The allergic contact dermatitis (CD) is a delayed-type (type 4) hypersensitivity reaction to immunogenic molecules or hapten in previously sensitized individuals. It comprises two phases: The sensitization phase and the elicitation phase. Sensitization happens when antigen-captured Langerhans cells migrate from the skin to lymph nodes and induce antigen-specific effector T cells. In the elicitation phase, the activated effector T cells release various chemical mediators, which produce antigen-specific inflammation.[2]
AD is a chronic inflammatory condition that affects 10–20% of the pediatric population.[3] It commonly presents with relapsing pruritic lesions characterized by erythema, oozing, crusting, scaling, and lichenification. Eyelid dermatitis and lip cheilitis are minor manifestations of AD. Due to disrupted skin barrier in atopic children, thin skin over the face, and chronic rubbing and scratching behavior in atopics, there are higher chances of eyelid and lip dermatitis. There has been an increased trend of various make-up and skin care routines among young adults and among young mothers due to growing social media outreach and influencer culture. A few commonly encountered products are moisturizers, cleansers, shampoos, toothpaste, cosmetics, sunscreens, and fragrances. Moisturizer, despite being the mainstay of treatment for AD, may cause hypersensitivity reactions because of its ingredients or vehicle.[4] Thiomersal is a common preservative found in most of the commercially available face creams, cosmetics, and antiseptic medications. Fragrances, including balsam of Peru, are found in a wide variety of consumer products such as serums, creams, lotions, soaps, shampoos, body wash, toothpaste, and perfumes. Nickel, which is a common sensitizer, is present in almost all types of fashionable jewelry, belt buckles, safety pins, hooks, buttons, watches, and optical frames, as well as in brown and red pigments of makeup products such as eye shadows.[5-8] In a previous study done with 114 pediatric patients by Beattie et al., they found nickel to be the most common allergen, followed by rubber chemicals, fragrance, cobalt, and lanolin.[9] However, in lip dermatitis, a North American study states that Fragrance and Balsam of Peru were the most relevant allergens.[10] School-going children indulge in various hobbies with materials such as crayons, paints, adhesives, latex, playing clay, slime, nail lacquers, and cement.[11] These materials usually contain colophony, hexamine, and potassium dichromate-like allergens that are often carried by the hands to the perioral and periorbital areas of the face.
Recurrent eczema over periorbital and perioral areas may indicate an atopic or allergic cause or maybe a combination of both. Despite the increasing prevalence, ACD is underreported in the pediatric population due to the reluctance in patch-testing in this age group. In our case series, there was the resolution of lesions without further relapse on the removal of the positive allergens, thereby pointing toward an allergic component.
Facial dermatitis in the form of eyelid eczema or cheilitis has an immense psychosocial impact, thereby altering the quality of life for both the child and the parent. Patch-testing is a vital diagnostic modality that can help identify the culprit allergen and can prevent further episodes by its careful avoidance. Our study emphasizes the requirement of patch testing for prompt diagnosis and management in such chronic cases.
Ethical approval
Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirms that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Prevalence of contact allergy in the general population: A systematic review and meta-analysis. Contact Dermatitis. 2019;80:77-85.
- [CrossRef] [PubMed] [Google Scholar]
- Contact dermatitis In: StatPearls. Treasure Island, FL: StatPearls Publishing; 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK459230 [Last accessed on 2023 Sep 04]
- [Google Scholar]
- Vehicles for drug delivery and cosmetic moisturizers: Review and comparison. Pharmaceutics. 2021;13:2012.
- [CrossRef] [PubMed] [Google Scholar]
- Eyelid dermatitis in patients referred for patch testing: Retrospective analysis of North American Contact Dermatitis Group data, 1994-2016. J Am Acad Dermatol. 2021;84:953-64.
- [CrossRef] [PubMed] [Google Scholar]
- Periorbital dermatitis: Causes, differential diagnoses and therapy. J Dtsch Dermatol Ges. 2010;8:159-66.
- [CrossRef] [PubMed] [Google Scholar]
- Patch tests in children with suspected allergic contact dermatitis: A prospective study and review of the literature. Dermatology. 2009;218:119-25.
- [CrossRef] [PubMed] [Google Scholar]
- Seven common allergen groups causing eyelid dermatitis: Education and avoidance strategies. Clin Ophthalmol. 2021;15:1477-90.
- [CrossRef] [PubMed] [Google Scholar]
- Patch-testing North American lip dermatitis patients: Data from the North American Contact Dermatitis Group, 2001 to 2004. Dermatitis. 2008;19:202-8.
- [CrossRef] [PubMed] [Google Scholar]
- Hidden risks in toys: A systematic review of pediatric toy contact dermatitis. Contact Dermatitis. 2020;82:265-71.
- [CrossRef] [PubMed] [Google Scholar]





