Translate this page into:
A rare presentation of pompholyx in a child mimicking bullous pemphigoid
*Corresponding author: Sudharani Chintagunta, Department of Dermatology, Venereology and Leprology, Gandhi Medical College, Hyderabad, Telangana, India. schintagunta@gmail.com
-
Received: ,
Accepted: ,
How to cite this article: Chittarvu K, Tejaswaroop M, Bhukya AK, Chintagunta S. A rare presentation of pompholyx in a child mimicking bullous pemphigoid. Indian J Skin Allergy. 2025;4:72-4. doi: 10.25259/IJSA_45_2024
Abstract
Pompholyx, or dyshidrotic eczema, an eczematous condition predominantly seen in adults, occasionally presents in children, where it can be mistaken for other bullous diseases, such as bullous pemphigoid (BP). This case report describes a rare and atypical presentation of pompholyx in a 7-year-old male who exhibited vesicular and bullous lesions on the palms, soles, and dorsae of the feet, mimicking BP. Histopathological examination showed spongiotic reaction and intraepidermal vesicle formation, and direct immunofluorescence was negative for immunoglobulin (Ig)G, IgA, IgM, and C3 deposits, ruling out BP and confirming a diagnosis of pompholyx. Treatment with systemic and topical corticosteroids and emollients led to rapid improvement, with complete resolution in 1 month. A 3-month follow-up showed no recurrence. This case emphasizes the diagnostic challenge of differentiating pompholyx from BP in pediatric patients due to clinical overlap. Accurate identification is essential, as management strategies differ significantly; misdiagnosis can lead to unnecessary immunosuppressive therapy. This report also highlights the need for increased awareness of atypical presentations of pompholyx in children to optimize patient outcomes and reduce treatment-related complications.
Keywords
Childhood bullous pemphigoid
Pediatric eczema
Pediatric pompholyx
Pompholyx
Pompholyx in children
INTRODUCTION
Pompholyx, also known as dyshidrotic eczema or dyshidrosis, is a form of eczema characterized by the sudden onset of small, intensely pruritic vesicles on the palms, sides of the fingers, and soles of the feet. Although it is more commonly seen in adults, pompholyx can occur in children, where it may present differently or be mistaken for other dermatological conditions, such as bullous pemphigoid (BP).[1] Given the clinical overlap between these two conditions, especially in pediatric populations, accurate diagnosis is critical to avoid unnecessary immunosuppressive treatment associated with BP.
We report a case of a 7-year-old male who presented with vesicular lesions resembling BP but was then diagnosed with pompholyx.
CASE REPORT
A 7-year-old boy presented with chief complaints of fluid-filled lesions over bilateral palms, fingers, soles, and dorsae of the feet for 2 weeks associated with intense itching. The lesions began as small, tense vesicles that progressively coalesced into larger bullae. The patient had no significant medical history, and no recent changes in medication, diet, or exposure to new allergens were reported. There was no family or personal history of atopy.
On examination, the patient had multiple clear vesicles and tense bullae with erythematous borders, a few crusted papules, and excoriations on the palms, fingers, soles, and dorsae of the feet [Figures 1 and 2]. The Nikolsky sign was negative, and no mucosal involvement was present. General and systemic examination was unremarkable. There was no clinical evidence of eczema, infection, or any findings suggestive of atopic dermatitis. Based on the clinical presentation, the differential diagnosis of dyshidrosiform pemphigus vulgaris, BP, and pompholyx were considered.
Routine blood tests were unremarkable. Serum immunoglobulin E (S.IgE) levels were normal. Skin biopsy from the bullous lesion over the dorsum of the right foot showed a spongiotic reaction pattern revealing epidermis with moderate orthokeratosis, moderate spongiosis, and intraepidermal vesicle. The upper dermis shows mild infiltrate of lymphocytes and occasional eosinophils around the vessels and adnexae with intraepidermal vesicle formation consistent with pompholyx [Figure 3a and b]. Direct immunofluorescence from the perilesional skin was negative for immunoglobulin (Ig)G, IgA, IgM, and C3 deposits, ruling out BP. The final diagnosis of pompholyx was confirmed. The patient was treated with a short course of systemic corticosteroids, topical corticosteroids, and emollients, leading to significant improvement in symptoms within 2 weeks. The lesions resolved completely by 1 month. Regular follow-up over the next 3 months showed no recurrence of the lesions.

- Multiple clear vesicles and tense bullae with erythematous borders, a few crusted papules, and excoriations on the palms, fingers, soles, and dorsae of the feet.

- Multiple clear vesicles and tense bullae with erythematous borders, a few crusted papules, and excoriations on the dorsum of the foot.
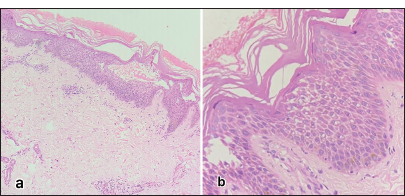
- (a) HPE ×10 shows epidermis with moderate orthokeratosis, moderate spongiosis, and intraepidermal vesicle. The basal layer is intact. The upper dermis shows mild infiltrate of lymphocytes and occasional eosinophils around the vessels and adnexae, (b) HPE ×40 shows epidermis with moderate orthokeratosis, moderate spongiosis, and intraepidermal vesicle. The basal layer is intact. The upper dermis shows mild infiltrate of lymphocytes and occasional eosinophils around the vessels and adnexae. HPE: Histopathological examination.
DISCUSSION
The prevalence of pompholyx in children is not well documented, but studies suggest that pompholyx accounts for a small percentage (1–5%) of pediatric eczema cases.[2,3] The exact etiology of pompholyx in children is not fully understood, but it is believed to be multifactorial. Triggers may include stress, allergic reactions, hyperhidrosis, and environmental factors such as heat and humidity. Genetic predisposition may also play a role, as children with a family history of atopic dermatitis or other forms of eczema may be more susceptible. However, pompholyx can also occur independently of other atopic conditions which was observed in this case.[4] Atopic dermatitis was ruled out according to the American Academy of Dermatology diagnostic criteria, family history of atopy was negative, and S.IgE levels were also normal.[5] The diagnosis of pompholyx in children is primarily clinical; however, certain atypical presentations, such as large bullae, warrant the need for biopsy. In the present case, the biopsy findings of spongiotic reaction pattern with intraepidermal vesicle formation, spongiosis, and mild-to-moderate perivascular lymphocytic infiltrate were consistent with pompholyx as opposed to BP, which shows subepidermal split with a superficial perivascular inflammatory infiltrate and numerous eosinophils. Eosinophils may be present in pompholyx also but are not as prominent as in BP.[1,6]
The differential diagnoses considered were allergic and irritant contact dermatitis, which were deemed unlikely due to the absence of identifiable triggers. Bullous dermatophyte infection was ruled out by a negative potassium hydroxide mount, whereas epidermolysis bullosa acquisita was excluded because the blisters were not trauma-induced and showed no recurrence. Dyshidrotiform pemphigus vulgaris was ruled out based on the absence of acantholytic cells in the Tzanck smear. The absence of honey-colored crusts and lack of response to antibiotics ruled out bullous impetigo, and the absence of family history combined with no evidence of mite excluded a diagnosis of scabies.
Each of these differential diagnoses has a distinct history and clinical, histological, and immunopathological features that aid in diagnosis. Proper identification and management depend on recognizing these unique aspects, supported by histopathology, microbiology, and immunofluorescence where appropriate. The occurrence of pompholyx in the pediatric age group, the severity of the presentation simulating BP, and the presence of the lesions over the dorsum of hands and feet make this case atypical. The other atypical presentations of pompholyx reported in the literature are summarized in Table 1.[7-10] A case series of dyshidrotic BP mimicking pompholyx in adults has been documented.[6] Although pompholyx and BP can present similarly, key differences in histopathology and immunofluorescence studies are crucial for accurate diagnosis.[6]
| Case | Patient profile | Initial misdiagnosis | Diagnostic challenges | Final diagnosis | Treatment | Outcome |
|---|---|---|---|---|---|---|
| Case 1: Atypical Pompholyx with Secondary Infection | A 15-year-old girl with Ebstein anomaly | Scabies | Recurrent pruritic pustules initially attributed to scabies | Pompholyx with secondary Staphylococcus and Klebsiella infections | Topical corticosteroids, emollients, antibiotics | Improvement with targeted therapy |
| Case 2: Palmar Lichen Nitidus Mimicking Pompholyx | A 12-year-old boy with vesicles on the right palm | Pompholyx | Pruritic, erythematous papules and vesicles resembling pompholyx | Palmar lichen nitidus | Topical corticosteroids, tacrolimus | Symptom improvement after correct diagnosis |
| Case 3: Photoinduced Pompholyx | Five patients (ages unspecified) with sun-exposed hands | Photosensitive dermatitis | Pruritic eruptions with erythematous papules linked to sun exposure | Photoinduced pompholyx | Topical corticosteroids, sun protection | Resolved withavoidance of triggers |
| Case 4: Vesico-Bullous Rash Misdiagnosed as Scabies | A 31-year-old male with vesicular rash on palms | Scabies | Pruritic rash and vesicles similar to scabies; delayed histopathology | Pompholyx | Topical corticosteroids, emollients | Improvement after correct diagnosis |
| Case 5: Unusual Presentation of Severe Pompholyx with Hemorrhagic Bullae[1] | A 25-year-old woman with severe hemorrhagic bullae over her hands and feet | Dyshidrotic eczema | Classic vesicular lesions progressed to hemorrhagic bullae over hands and feet; resistant to initial topical steroids | Severe pompholyx with hemorrhagic bullae | Systemic corticosteroids | Improvement after systemic treatment |
CONCLUSION
We conclude that, the differentiation between Pompholyx and Bullous Pemphigoid is critical because the management strategies differ significantly. Early and appropriate diagnosis can prevent unnecessary treatment and improve patient outcomes.
Ethical approval
The Institutional Review Board approval is not required.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent.
Conflicts of interest
There are no conflicts of interest.
Use of artificial intelligence (AI)-assisted technology for manuscript preparation
The authors confirm that there was no use of artificial intelligence (AI)-assisted technology for assisting in the writing or editing of the manuscript and no images were manipulated using AI.
Financial support and sponsorship: Nil.
References
- Unusual presentation of severe pompholyx. Indian Dermatol Online J. 2014;5:S48-9.
- [CrossRef] [PubMed] [Google Scholar]
- The U.K working party's diagnostic criteria for atopic dermatitis. III. Independent hospital validation. Br J Dermatol. 1994;131:406-16.
- [CrossRef] [PubMed] [Google Scholar]
- The clinical spectrum of atopic dermatitis. J Allergy Clin Immunol. 1999;104:S87-98.
- [CrossRef] [PubMed] [Google Scholar]
- A 3-year causative study of pompholyx in 120 patients. Arch Dermatol. 2007;143:1504-8.
- [CrossRef] [PubMed] [Google Scholar]
- Nomenclature and clinical phenotypes of atopic dermatitis. Ther Adv Chronic Dis. 2021;12:20406223211002979.
- [CrossRef] [PubMed] [Google Scholar]
- Dyshidrosiform bullous pemphigoid. Medicina (Kaunas). 2021;57:398.
- [CrossRef] [PubMed] [Google Scholar]
- Atypical pompholyx presentation of secondary Staphyloccoccus and Klebsiella infections in a patient with premorbid Ebstein anomaly: A case report. Asian Pac J Trop Med. 2023;16:45-8.
- [CrossRef] [Google Scholar]
- A case of palmar lichen nitidus presenting as a clinical feature of pompholyx. Ann Dermatol. 2010;22:235-7.
- [CrossRef] [PubMed] [Google Scholar]
- Photoinduced pompholyx: A report of 5 cases. J Am Acad Dermatol. 2004;50:55-60.
- [CrossRef] [PubMed] [Google Scholar]
- Vesico-bullous rash caused by pompholyx eczema. BMJ Case Rep. 2012;2012:bcr1120115135.
- [CrossRef] [PubMed] [Google Scholar]






